Tonsillar bleeding following mechanical trauma represents a concerning medical scenario that requires immediate attention and proper management. When individuals attempt to remove tonsil stones or examine their throat using fingers, cotton buds, or other implements, they risk causing significant damage to the delicate vascular structures within the palatine tonsils. This type of injury can range from minor surface abrasions to serious haemorrhage requiring emergency intervention. Understanding the appropriate response to tonsillar bleeding is crucial for preventing complications and ensuring optimal patient outcomes. The rich blood supply to the tonsillar region means that even seemingly minor trauma can result in substantial bleeding that may appear alarming to patients and their families.
Understanding tonsillar trauma and haemorrhage mechanisms
Anatomical structure of palatine tonsils and vascular supply
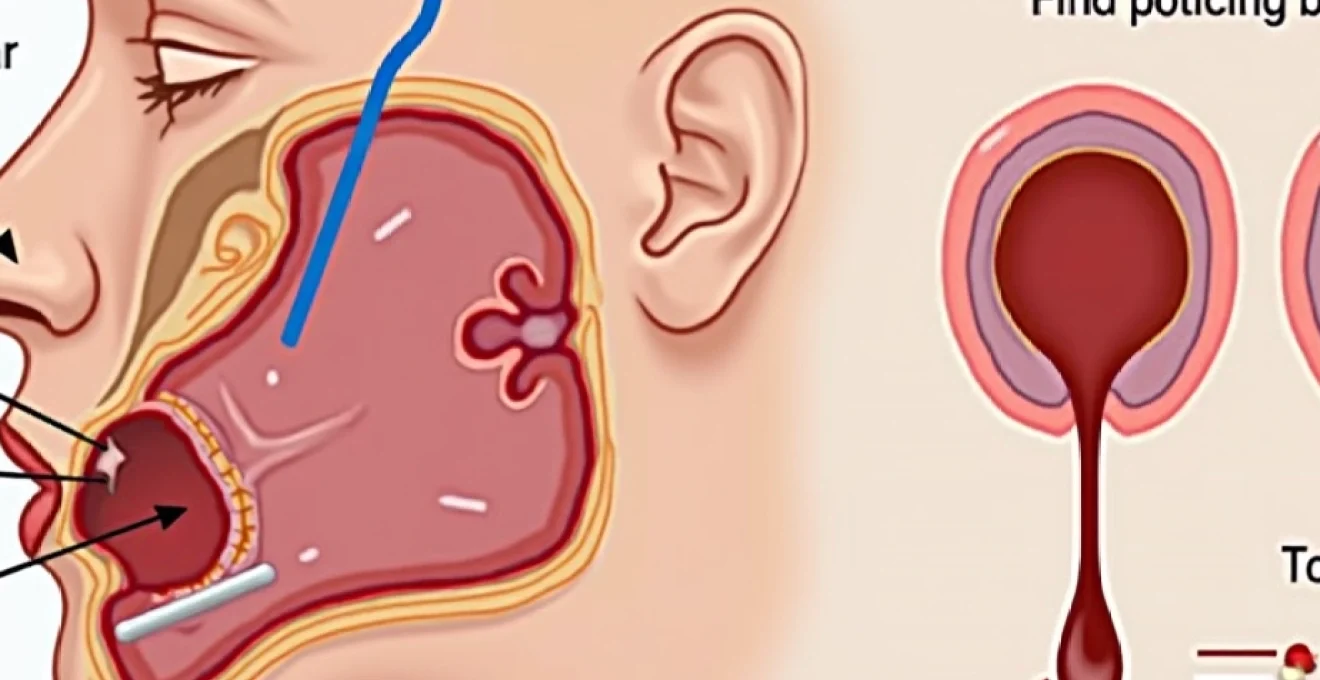
The palatine tonsils occupy a strategic position within the oropharynx, nestled between the anterior and posterior tonsillar pillars. These lymphoid structures possess an exceptionally rich vascular network that makes them particularly susceptible to bleeding when traumatised. The primary arterial supply derives from the tonsillar branch of the facial artery, supplemented by contributions from the ascending pharyngeal artery, the greater palatine artery, and branches of the lingual artery. This extensive vascularisation serves the tonsils’ immune function but creates significant bleeding risk during mechanical injury.
The venous drainage follows a similarly complex pattern, with blood flowing through the tonsillar veins into the pharyngeal venous plexus before ultimately reaching the internal jugular vein. The presence of numerous small vessels throughout the tonsillar crypts and surface epithelium means that even superficial trauma can cause impressive bleeding that may appear disproportionate to the actual injury sustained.
Pathophysiology of mechanical tonsillar injury
Mechanical trauma to the tonsils typically occurs when individuals attempt to dislodge tonsil stones or examine their throat using inappropriate instruments. The delicate nature of tonsillar tissue means that relatively minor force can cause significant disruption to surface vessels and deeper vascular structures. When you apply pressure or scraping motions to the tonsillar surface, the resulting injury often involves multiple small vessels rather than a single large bleeding source.
The bleeding pattern following tonsillar trauma typically manifests as continuous oozing rather than pulsatile arterial haemorrhage, though more significant injuries can involve deeper arterial structures. The body’s natural haemostatic mechanisms may be overwhelmed in cases of extensive surface trauma, particularly when multiple crypts are damaged simultaneously. Understanding this mechanism helps explain why tonsillar bleeding can appear more severe than other oral injuries of similar magnitude .
Classification of tonsillar bleeding severity using the windfuhr scale
Medical professionals utilise the Windfuhr scale to categorise tonsillar haemorrhage severity and guide treatment decisions. Grade I bleeding involves minor oozing that stops spontaneously within minutes and requires no intervention beyond observation. Grade II haemorrhage presents as more persistent bleeding that may require basic first aid measures but typically resolves with conservative management within 30 minutes.
Grade III bleeding represents a more serious scenario where active haemorrhage continues despite first aid measures and requires professional medical intervention. Grade IV haemorrhage constitutes a medical emergency , characterised by profuse bleeding that threatens airway patency or causes haemodynamic instability. This classification system helps determine the urgency of medical intervention and guides treatment protocols for healthcare providers managing tonsillar bleeding cases.
Risk factors for spontaneous tonsillar haemorrhage
Several factors can predispose individuals to increased bleeding risk following tonsillar trauma. Patients with underlying bleeding disorders such as haemophilia, von Willebrand disease, or platelet dysfunction face significantly elevated haemorrhage risk even from minor tonsillar injuries. Medications that affect coagulation, including warfarin, clopidogrel, and novel oral anticoagulants, can dramatically increase bleeding severity and duration.
Chronic tonsillar inflammation or recent upper respiratory tract infections can make tonsillar tissue more friable and prone to bleeding when traumatised. Individuals with a history of recurrent tonsillitis often have more prominent vascular networks that increase bleeding risk . Age-related factors also play a role, with elderly patients experiencing slower healing and increased complications from tonsillar trauma due to reduced regenerative capacity and often concurrent medical conditions that impair normal haemostatic function.
Immediate first aid management for tonsillar bleeding
Primary haemostasis techniques and direct pressure application
The initial management of tonsillar bleeding focuses on achieving primary haemostasis through direct pressure application and positioning techniques. When you encounter tonsillar bleeding, the first priority involves applying gentle but firm pressure to the bleeding site using clean gauze or a cloth. Unlike external wounds, direct pressure on tonsils requires careful technique to avoid further trauma while achieving effective compression of bleeding vessels.
Instruct the patient to tilt their head forward slightly and apply pressure using rolled gauze held against the affected tonsil for 10-15 minutes continuously. Avoid the temptation to frequently check if bleeding has stopped, as this disrupts clot formation . If initial pressure proves ineffective, consider using a clean cloth soaked in cold water to provide both pressure and cooling effects simultaneously. The key to successful direct pressure lies in maintaining consistent, gentle compression without causing additional trauma to the already injured tissue.
Cold therapy protocols and vasoconstriction methods
Cold therapy serves as an effective adjunct to direct pressure in managing tonsillar bleeding by promoting vasoconstriction and reducing local inflammation. Ice chips or crushed ice wrapped in a thin cloth can be applied to the external neck area over the tonsillar region to provide systemic cooling effects. However, placing ice directly against the tonsils may cause additional trauma and should be avoided.
Cold water gargles represent a more practical approach for achieving local vasoconstriction. Prepare cold saline solution using one teaspoon of salt dissolved in 240ml of cold water, and have the patient perform gentle gargling motions for 30-60 seconds at a time. This technique provides both mechanical cleansing of blood clots and therapeutic cooling to promote vessel constriction. Repeat cold therapy applications every 15-20 minutes during the first hour following injury to maximise vasoconstrictor effects and reduce overall bleeding severity.
Patient positioning and airway management considerations
Proper patient positioning plays a crucial role in managing tonsillar bleeding safely while preventing aspiration of blood into the respiratory tract. Position the patient in an upright, forward-leaning posture that allows blood to drain from the mouth rather than pooling in the posterior pharynx. This positioning reduces aspiration risk and provides better visualisation of the bleeding source for ongoing assessment.
Encourage the patient to spit out accumulated blood rather than swallowing it, as ingested blood can cause nausea and vomiting that may complicate management.
Maintaining clear airways remains the paramount concern in tonsillar bleeding management, as blood accumulation can rapidly compromise breathing
. Monitor the patient’s ability to speak clearly and swallow normally, as deterioration in these functions may indicate increasing oropharyngeal blood accumulation or developing airway compromise requiring immediate medical intervention.
When to apply topical haemostatic agents
Topical haemostatic agents can provide valuable assistance in controlling tonsillar bleeding when conventional measures prove insufficient. Over-the-counter products containing tranexamic acid or aluminium chloride may help promote clot formation and vessel constriction when applied directly to bleeding sites. However, these agents should only be used when you can clearly visualise the bleeding source and apply them safely without risk of aspiration.
Commercial haemostatic gauze products designed for oral use offer another option for persistent bleeding. These specialised materials contain clotting factors that enhance the body’s natural coagulation mechanisms. Apply these products with gentle pressure for the manufacturer’s recommended duration , typically 2-5 minutes, while maintaining proper patient positioning to prevent aspiration. Be aware that topical agents may temporarily increase local discomfort and should not delay seeking professional medical care if bleeding continues despite their use.
Medical assessment and clinical evaluation procedures
Professional medical evaluation becomes necessary when first aid measures fail to control tonsillar bleeding within 30 minutes or when bleeding recurs repeatedly after initial cessation. Healthcare providers conduct systematic assessments beginning with vital sign monitoring to detect any signs of haemodynamic compromise. Blood pressure, heart rate, and oxygen saturation measurements provide crucial information about the patient’s physiological response to blood loss and guide treatment intensity decisions.
The clinical examination focuses on determining bleeding severity, location, and underlying causes. Direct visualisation using appropriate lighting and instruments allows healthcare providers to identify specific bleeding vessels and assess the extent of tonsillar trauma. Examination techniques must balance the need for thorough assessment with the risk of provoking additional bleeding through excessive manipulation . Providers evaluate for signs of active arterial bleeding, venous oozing, or mixed bleeding patterns that influence treatment selection.
Laboratory investigations may be warranted depending on bleeding severity and patient history. Complete blood count measurements help assess the degree of blood loss and identify any underlying haematological abnormalities. Coagulation studies including prothrombin time, activated partial thromboplastin time, and international normalised ratio provide essential information about the patient’s clotting function.
Patients with known bleeding disorders or those taking anticoagulant medications require particularly careful evaluation and may need additional specialist consultation
. The medical assessment process guides treatment decisions and helps identify patients requiring more intensive interventions or monitoring.
Professional treatment options for persistent tonsillar haemorrhage
Electrocautery and bipolar diathermy techniques
Electrocautery represents the gold standard for controlling persistent tonsillar bleeding in clinical settings. Bipolar diathermy techniques offer precise control over bleeding vessels while minimising thermal damage to surrounding healthy tissue. This approach allows healthcare providers to selectively coagulate specific bleeding points without causing extensive tissue destruction that could impair healing or increase infection risk.
The procedure requires appropriate anaesthesia, typically achieved through topical application of lidocaine-based solutions or infiltration anaesthesia around the bleeding site. Careful technique ensures effective haemostasis while preserving maximal tonsillar function . Modern electrocautery units provide adjustable power settings that allow customisation based on vessel size and bleeding intensity. The immediate effectiveness of this technique makes it particularly valuable for patients with persistent bleeding that has failed to respond to conservative measures.
Chemical cauterisation using silver nitrate application
Silver nitrate cauterisation offers an alternative approach for managing tonsillar bleeding, particularly in cases where electrocautery equipment is unavailable or inappropriate. This technique involves direct application of silver nitrate sticks to bleeding vessels, causing immediate chemical coagulation through protein precipitation. The method requires precise application to bleeding sites while avoiding contact with healthy tissue that could result in unnecessary tissue destruction.
Healthcare providers must exercise caution when using silver nitrate near tonsillar tissue due to the risk of excessive tissue damage or inadvertent application to non-bleeding areas. The technique works best for localised bleeding from small vessels rather than diffuse oozing from multiple sites . Patients typically experience immediate cessation of bleeding following successful silver nitrate application, though some temporary discomfort and tissue discolouration may occur at treatment sites. This method provides effective haemostasis while avoiding the need for more invasive procedures in appropriately selected cases.
Suture ligation methods for vessel control
Suture ligation techniques become necessary when bleeding originates from larger vessels that cannot be controlled through cauterisation methods alone. This approach involves the precise placement of absorbable sutures around bleeding vessels or areas of tonsillar trauma to achieve mechanical compression and vessel occlusion. The technique requires considerable skill and experience due to the complex anatomy of the tonsillar region and the proximity of important structures.
Healthcare providers utilise fine absorbable sutures, typically 4-0 or 5-0 polyglactin or chromic gut, to minimise tissue reaction while providing adequate tensile strength for effective haemostasis. Suture placement must be carefully planned to avoid damage to adjacent structures while ensuring complete vessel occlusion . This technique often provides more durable haemostasis than cauterisation methods alone and may be preferred in cases where recurrent bleeding is a concern. The procedure typically requires local or regional anaesthesia and may be performed in outpatient settings for stable patients.
Emergency tonsillectomy indications and procedures
Emergency tonsillectomy represents the definitive treatment for life-threatening tonsillar haemorrhage that cannot be controlled through less invasive measures. This procedure becomes necessary when bleeding threatens airway patency, causes haemodynamic instability, or fails to respond to multiple attempts at conservative management.
The decision to proceed with emergency tonsillectomy requires careful consideration of surgical risks versus the ongoing bleeding threat
. Patient factors including age, comorbidities, and coagulation status all influence the risk-benefit analysis.
The surgical approach for emergency tonsillectomy often differs from elective procedures due to the presence of active bleeding and potentially compromised anatomy. Surgeons must achieve rapid, effective haemostasis while ensuring complete removal of tonsillar tissue that could serve as a source of recurrent bleeding. Advanced techniques including harmonic scalpel technology or coblation methods may be employed to minimise thermal tissue damage while achieving reliable haemostasis. Post-operative monitoring requirements are typically more intensive following emergency procedures, with particular attention to signs of recurrent bleeding or airway compromise.
Complications and warning signs requiring urgent intervention
Recognition of complications following tonsillar bleeding enables timely intervention that can prevent life-threatening scenarios. Airway compromise represents the most serious immediate complication, occurring when blood accumulation or tissue swelling obstructs normal breathing patterns. Early warning signs include stridor, difficulty speaking, increased respiratory effort, or changes in voice quality that suggest developing upper airway obstruction. Any signs of respiratory distress require immediate emergency medical attention regardless of apparent bleeding severity .
Haemodynamic instability can develop rapidly in cases of significant blood loss, particularly in children or elderly patients with limited physiological reserves. Signs of shock including tachycardia, hypotension, altered mental status, or decreased urine output indicate the need for immediate fluid resuscitation and urgent medical intervention. Patients may initially compensate for blood loss through increased heart rate and peripheral vasoconstriction, making early recognition crucial for preventing progression to irreversible shock states.
Aspiration pneumonia represents a delayed complication that can occur when patients inadvertently inhale blood during episodes of tonsillar bleeding. This risk is particularly elevated in patients with altered consciousness, neuromuscular disorders, or gastroesophageal reflux disease. Prevention strategies include maintaining appropriate positioning, encouraging expectoration rather than swallowing of blood, and seeking immediate medical attention for patients showing signs of respiratory distress following bleeding episodes. Healthcare providers must maintain high suspicion for aspiration complications, particularly in vulnerable patient populations who may not exhibit typical symptoms immediately following blood aspiration events.
Infection complications can develop at tonsillar injury sites, particularly when foreign material was introduced during the initial trauma or when tissue devitalisation has occurred. Signs of secondary infection include increasing pain, fever, purulent discharge, or worsening swelling several days after the initial bleeding episode. These complications require antibiotic therapy and may necessitate additional interventions to drain infected collections or remove necrotic tissue that could serve as a nidus for ongoing infection.
Prevention strategies and Post-Bleeding care management
Effective prevention of tonsillar trauma focuses on education about safe oral hygiene practices and appropriate methods for managing tonsil-related concerns. Patients should understand that attempting to remove tonsil stones using fingers, toothpicks, or other rigid implements carries significant bleeding risk and potential for serious injury. Professional evaluation and treatment provide safer alternatives for addressing persistent tonsillar issues . Healthcare providers should educate patients about recognising signs that warrant professional attention rather than attempting self-treatment of tonsillar problems.
Post-bleeding care management focuses on promoting healing while preventing recurrent episodes or complications. Patients should maintain soft diet restrictions for 24-48 hours following bleeding episodes to minimise mechanical trauma to healing tissues. Adequate hydration helps maintain optimal blood viscosity and supports natural healing processes. Avoid hot liquids, carbonated beverages, and acidic foods that could irritate healing tonsillar tissue or promote bleeding recurrence through chemical irritation.
Follow-up care protocols should be established based on bleeding severity and underlying risk factors. Patients with significant bleeding episodes require scheduled reassessment within 24-48 hours to ensure proper healing and identify any developing complications. Those with
underlying bleeding disorders may require longer follow-up periods and coordination with haematology specialists to optimise their coagulation management before any future procedures. Regular oral hygiene education helps patients maintain tonsillar health and reduces the likelihood of developing conditions that might tempt them to attempt self-treatment.
Medication management forms a crucial component of post-bleeding care, particularly for patients taking anticoagulant or antiplatelet medications. Healthcare providers must balance the need to prevent thrombotic complications with the risk of recurrent bleeding when making decisions about resuming these medications. Close collaboration with prescribing physicians ensures optimal timing for medication resumption based on individual risk factors. Pain management should focus on medications that do not impair platelet function, avoiding aspirin-containing products that could increase bleeding risk during the healing period.
Patient education materials should emphasise warning signs that require immediate medical attention, including renewed bleeding, increasing pain, difficulty swallowing, or signs of infection. Establishing clear communication pathways between patients and healthcare providers facilitates prompt intervention when complications arise. Many healthcare systems now utilise telephone triage services or secure messaging platforms that allow patients to report concerns quickly and receive appropriate guidance about the need for in-person evaluation.
Long-term prevention strategies may include addressing underlying conditions that predispose patients to tonsillar problems. Chronic sinusitis, gastroesophageal reflux disease, and allergic rhinitis can all contribute to tonsillar inflammation and stone formation that might prompt patients to attempt self-treatment. Comprehensive management of these conditions reduces the likelihood of tonsillar complications and subsequent trauma. Regular dental care and professional oral hygiene maintenance also play important roles in preventing conditions that might lead patients to manipulate their tonsillar tissue inappropriately.
For patients with recurrent tonsil stone formation, healthcare providers should discuss safe removal techniques and professional treatment options that eliminate the need for dangerous self-treatment attempts. Water irrigation devices designed for oral use, regular salt water gargles, and scheduled professional cleanings can help manage tonsil stones safely without risking traumatic bleeding. Patient education about when to seek professional help rather than attempting self-treatment represents one of the most effective prevention strategies available.