Tonsilloliths, commonly known as tonsil stones, represent a fascinating yet troublesome phenomenon where calcified debris accumulates within the crypts of palatine tonsils. While most individuals experience these formations as merely cosmetic inconveniences accompanied by halitosis, a subset of patients encounters a more concerning complication: haemorrhage from the tonsillar tissue itself. The occurrence of bleeding associated with tonsil stones involves complex pathophysiological mechanisms that extend far beyond simple mechanical irritation, encompassing bacterial biofilm formation, mineralisation processes, and inflammatory cascades that compromise the delicate vascular architecture of tonsillar tissue.
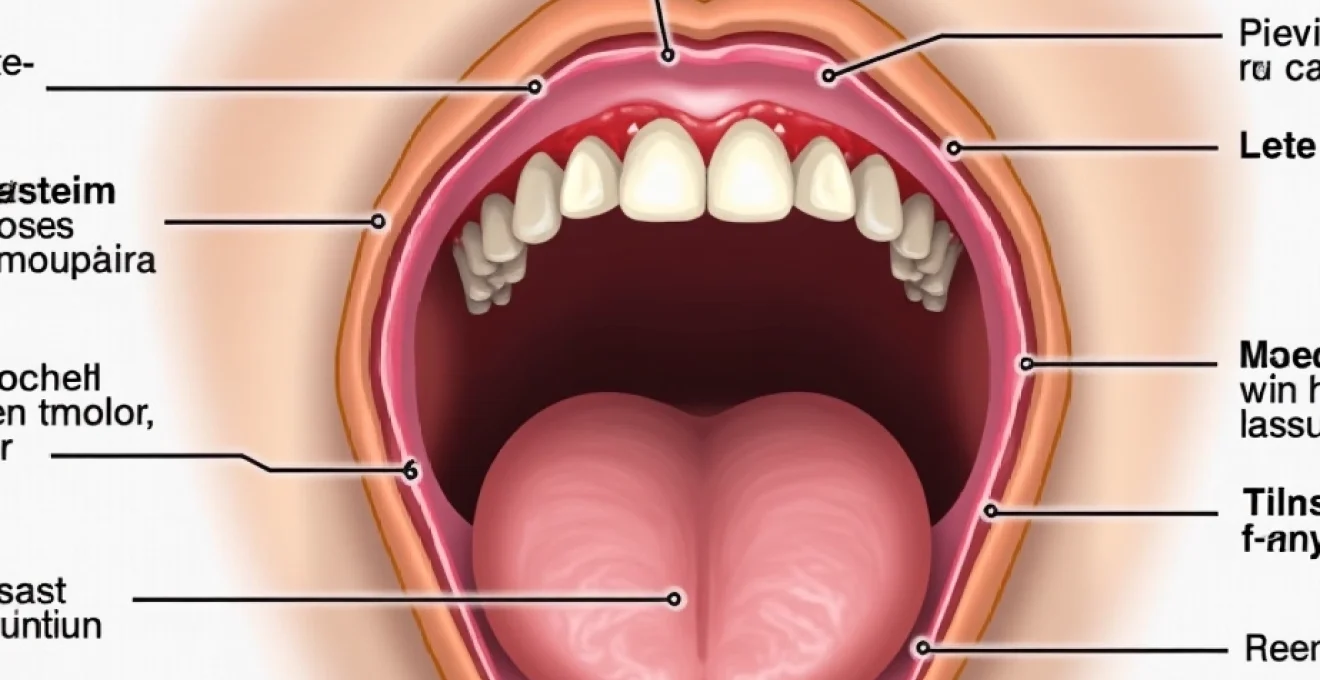
Understanding the intricate relationship between tonsillolith formation and subsequent bleeding episodes requires examination of multiple contributing factors. The palatine tonsils, with their extensive cryptic architecture and rich vascular supply, create an environment where calcified deposits can exert significant pressure on surrounding tissues while simultaneously fostering bacterial colonisation. This combination of mechanical stress and infectious burden establishes conditions conducive to vascular compromise and subsequent haemorrhagic episodes that can range from minor surface bleeding to more substantial haemorrhage requiring medical intervention.
Pathophysiology of Tonsillolith-Induced haemorrhage in palatine tonsils
The development of bleeding secondary to tonsil stones involves a complex interplay of mechanical, inflammatory, and infectious processes that compromise the structural integrity of tonsillar tissue. The palatine tonsils possess a unique architecture characterised by deep crypts lined with stratified squamous epithelium, creating numerous recesses where debris can accumulate and subsequently calcify. This cryptic anatomy, while serving important immunological functions, predisposes certain individuals to tonsillolith formation and associated complications including haemorrhage.
Cryptic epithelium erosion from calcium phosphate deposits
The initial stage of tonsillolith-related bleeding typically begins with erosion of the cryptic epithelium caused by accumulated calcium phosphate deposits. These calcified masses, composed primarily of calcium phosphate crystals interspersed with organic debris, exert continuous pressure against the delicate epithelial lining of tonsillar crypts. Over time, this persistent mechanical stress leads to epithelial thinning, ulceration, and eventual exposure of the underlying lamina propria where numerous capillaries reside. The process resembles a slow-motion pressure necrosis, where the hard, irregular surfaces of tonsilloliths gradually wear through the protective epithelial barrier, exposing vascular structures to potential trauma.
Capillary network disruption in tonsillar parenchyma
The rich capillary network within tonsillar parenchyma becomes increasingly vulnerable as tonsilloliths expand and exert pressure on surrounding tissues. The palatine tonsils receive blood supply from multiple sources, creating an extensive microvascular network that can be easily disrupted by mechanical pressure or inflammatory processes. When tonsil stones reach sufficient size, they compress these delicate vessels, leading to localised ischaemia followed by reactive hyperaemia upon pressure relief. This cycle of ischaemia-reperfusion creates conditions conducive to vessel wall weakening and subsequent rupture, particularly in individuals with underlying coagulopathies or those taking anticoagulant medications.
Inflammatory cascade response to biofilm accumulation
The presence of tonsilloliths triggers a robust inflammatory response that significantly contributes to bleeding risk through multiple mechanisms. Calcified debris provides an ideal substrate for bacterial biofilm formation, leading to chronic inflammation characterised by increased capillary permeability, vasodilation, and infiltration of inflammatory cells. This inflammatory milieu releases various mediators including histamine, prostaglandins, and cytokines that further compromise vascular integrity. The chronic nature of this inflammatory response means that even minor mechanical trauma can result in disproportionate bleeding due to the friable, hyperaemic state of the surrounding tissues.
Mechanical trauma from sharp tonsillolith edges
The irregular, crystalline structure of mature tonsilloliths creates sharp edges and rough surfaces that can directly lacerate surrounding tissues during normal physiological processes such as swallowing, coughing, or speaking. Unlike smooth foreign bodies that might be tolerated within tissue spaces, tonsil stones develop jagged contours as different mineral components crystallise at varying rates and patterns. These sharp projections act as microscopic surgical instruments, creating small but persistent wounds in the tonsillar tissue that may bleed intermittently. The continuous movement of the tonsils during normal oral functions ensures that these traumatic interactions occur repeatedly, preventing adequate healing and perpetuating the bleeding tendency.
Bacterial biofilm formation and vascular compromise mechanisms
The relationship between bacterial colonisation of tonsilloliths and subsequent bleeding represents a critical aspect of this condition that extends beyond simple mechanical irritation. Tonsil stones provide an ideal environment for bacterial biofilm formation due to their porous structure, protective location within tonsillar crypts, and continuous exposure to oral flora. These bacterial communities not only contribute to the characteristic malodour associated with tonsilloliths but also actively participate in tissue destruction through the production of various enzymes and toxins that compromise vascular integrity and promote bleeding episodes.
The complex ecosystem within tonsillolith biofilms creates a perfect storm of mechanical pressure and biochemical assault on surrounding tonsillar tissues, leading to progressive vascular compromise and increased bleeding risk.
Streptococcus pyogenes colonisation in tonsillar crypts
Streptococcus pyogenes , a gram-positive bacterium commonly associated with pharyngeal infections, frequently colonises tonsillolith surfaces where it contributes to tissue damage through multiple mechanisms. This pathogen produces numerous virulence factors including streptolysin O and S, which directly damage host cell membranes and compromise capillary integrity. Additionally, S. pyogenes secretes hyaluronidase, often termed “spreading factor,” which breaks down hyaluronic acid in connective tissue matrices, facilitating bacterial spread and weakening tissue architecture. The presence of this organism within tonsillolith biofilms creates localised areas of intense inflammatory activity that predispose surrounding vessels to rupture and bleeding.
Anaerobic fusobacterium nucleatum proliferation patterns
The anaerobic environment within deep tonsillar crypts harboring tonsilloliths provides optimal conditions for Fusobacterium nucleatum proliferation. This gram-negative anaerobe possesses unique adhesive properties that allow it to bridge different bacterial species within biofilm communities, creating stable, resilient microbial ecosystems. F. nucleatum produces various proteolytic enzymes that degrade collagen and elastin in blood vessel walls, directly contributing to vascular fragility and bleeding tendency. The organism’s ability to invade host epithelial cells and induce inflammatory responses further compounds tissue damage, creating a cycle of destruction that compromises hemostatic mechanisms and promotes persistent bleeding episodes.
Prevotella Intermedia-Mediated tissue degradation
Prevotella intermedia , another anaerobic gram-negative bacterium commonly isolated from tonsillolith specimens, contributes significantly to bleeding through its extensive arsenal of tissue-degrading enzymes. This organism produces collagenases, elastases, and other proteases that systematically break down extracellular matrix components essential for maintaining vascular integrity. The bacterium’s preference for haem-containing compounds drives it to actively seek out and colonise areas of minor bleeding, creating a positive feedback loop where bleeding attracts more bacteria, leading to increased tissue damage and further bleeding. This self-perpetuating cycle explains why some individuals experience recurrent bleeding episodes from tonsillolith sites.
Haemophilus influenzae endothelial invasion pathways
Haemophilus influenzae , while more commonly associated with respiratory tract infections, can establish residence within tonsillolith biofilms where it employs sophisticated mechanisms to invade endothelial cells lining tonsillar capillaries. The organism’s ability to undergo phase variation allows it to adapt rapidly to the unique microenvironment within calcified deposits, expressing different surface antigens that facilitate tissue invasion. Once established within endothelial cells, H. influenzae triggers inflammatory cascades that compromise tight junctions between cells, increase vascular permeability, and predispose to bleeding. The bacterium’s production of immunoglobulin A proteases further undermines local immune defenses, allowing persistent colonisation and ongoing tissue damage.
Mineralisation process contributing to tissue laceration
The progressive mineralisation of organic debris within tonsillar crypts transforms initially soft, malleable deposits into hard, crystalline structures capable of causing significant mechanical trauma to surrounding tissues. This transformation involves multiple mineral components that deposit in layers over time, creating increasingly complex and potentially harmful structures. Understanding the specific minerals involved and their deposition patterns provides insight into why certain tonsilloliths are more likely to cause bleeding than others, and how the timing of intervention might influence outcomes.
Hydroxyapatite crystal formation in debris matrix
Hydroxyapatite, the primary mineral component of tooth enamel and bone, represents the predominant crystalline phase in mature tonsilloliths. The formation of hydroxyapatite crystals within the organic matrix of accumulated debris creates exceptionally hard surfaces that can rival dental enamel in terms of mechanical properties. These crystals typically form in a radial pattern from nucleation sites within the debris mass, creating sharp, needle-like projections that extend outward toward surrounding tissues. The process is facilitated by the alkaline pH environment created by bacterial metabolism within the developing stone, which favours calcium phosphate precipitation. As these crystals grow and mature, they create increasingly dangerous sharp edges capable of lacerating delicate tonsillar tissues during normal oral movements.
Magnesium ammonium phosphate deposition mechanics
Magnesium ammonium phosphate, also known as struvite, forms secondary deposits within tonsilloliths under specific pH and ionic conditions created by bacterial metabolism. This mineral tends to precipitate in areas of high ammonia concentration, typically produced by urease-positive bacteria within the biofilm community. Struvite crystals exhibit a characteristic coffin-like shape with sharp edges and corners that can cause significant tissue trauma. The formation of these crystals often occurs in discrete layers alternating with organic material, creating a laminated structure that can fragment along crystal planes, producing sharp-edged fragments that act as microscopic surgical blades against surrounding tissues. The presence of struvite within tonsilloliths significantly increases their potential for causing laceration and subsequent bleeding.
Calcium carbonate accumulation and surface roughening
Calcium carbonate deposition occurs primarily in the outer layers of tonsilloliths, where exposure to carbon dioxide from respiration and bacterial fermentation creates conditions favourable for carbonate precipitation. While individually less sharp than phosphate crystals, calcium carbonate deposits contribute to overall surface roughening that increases the abrasive potential of tonsil stones. The mineral tends to form in irregular, botryoidal patterns that create a highly textured surface capable of causing chronic irritation and microtrauma to surrounding epithelium. This continuous low-level trauma maintains inflammatory conditions that keep tissues friable and prone to bleeding, even in the absence of acute mechanical injury.
Organic matrix calcification timeline and hardness development
The transformation of soft organic debris into calcified, potentially dangerous tonsilloliths follows a predictable timeline that influences both the likelihood of bleeding and the severity of associated complications. Initial mineralisation typically begins within 2-4 weeks of debris accumulation, starting with calcium phosphate precipitation around bacterial biofilms and cellular debris. Over subsequent months, the progressive incorporation of additional minerals increases both the size and hardness of the developing stone. Mature tonsilloliths can achieve Mohs hardness values comparable to fossilised materials, making them capable of causing significant tissue damage. Understanding this timeline is crucial for clinicians, as early intervention can prevent the development of hard, potentially harmful stones that pose increased bleeding risks.
Chronic tonsillitis exacerbating haemorrhagic episodes
The presence of tonsilloliths frequently coincides with chronic tonsillitis, creating a synergistic relationship that significantly amplifies bleeding risk through multiple pathophysiological mechanisms. Chronic inflammatory conditions within the palatine tonsils alter the local microenvironment in ways that both promote tonsillolith formation and increase the likelihood of haemorrhagic complications. The persistent inflammatory state characteristic of chronic tonsillitis leads to structural changes in tonsillar tissue that compromise natural hemostatic mechanisms while simultaneously creating conditions that favour bacterial colonisation and stone formation.
Chronic tonsillitis induces significant architectural changes in tonsillar tissue, including epithelial hyperplasia, submucosal fibrosis, and vascular remodelling that collectively increase bleeding susceptibility. The inflammatory process leads to increased capillary density and vessel fragility, while simultaneously impairing normal coagulation cascades through the production of inflammatory mediators that interfere with platelet aggregation and fibrin formation. These changes create a tissue environment where even minor trauma from tonsilloliths can result in disproportionate bleeding episodes that may be difficult to control using standard hemostatic measures.
The cyclical relationship between tonsillolith presence and chronic inflammation creates a self-perpetuating cycle of tissue damage and bleeding risk. Calcified deposits provide persistent antigenic stimulation that maintains chronic inflammatory responses, while the inflammatory environment promotes further stone formation through altered pH conditions and increased debris production from damaged epithelial cells. This cycle is particularly problematic because it tends to worsen over time, with larger stones causing more tissue damage and inflammation, leading to conditions that favour the formation of additional stones and increased bleeding complications.
Chronic tonsillitis creates a perfect storm of vascular fragility, impaired hemostasis, and persistent antigenic stimulation that transforms normally benign tonsilloliths into potential sources of significant bleeding complications.
The management of bleeding tonsilloliths in the context of chronic tonsillitis requires addressing both the mechanical presence of calcified deposits and the underlying inflammatory process. Standard approaches to tonsil stone removal may be inadequate or even dangerous in chronically inflamed tissues, as the altered vascular architecture increases the risk of significant haemorrhage during extraction attempts. Additionally, the persistent inflammatory environment often leads to rapid reformation of stones following removal, necessitating more definitive interventions such as cryptolysis or tonsillectomy to achieve lasting resolution of bleeding episodes.
Mechanical extraction trauma and iatrogenic bleeding
Attempts to remove tonsilloliths through mechanical extraction represent a significant cause of bleeding complications, particularly when performed by untrained individuals using improvised instruments or inappropriate techniques. The delicate nature of chronically inflamed tonsillar tissue, combined with the often deep embedding of calcified stones within cryptic recesses, creates conditions where extraction attempts frequently result in tissue trauma and subsequent bleeding. Understanding the mechanisms of extraction-related injury is crucial for both patients attempting self-removal and healthcare providers performing professional stone extraction procedures.
The most common mechanism of extraction-related bleeding involves direct trauma to the cryptic epithelium and underlying vascular structures during attempts to dislodge embedded stones. Tonsilloliths often become firmly anchored within cryptic recesses through a combination of mechanical wedging and adhesion to surrounding tissues through biofilm formation. Forceful extraction attempts using cotton swabs, dental instruments, or other improvised tools frequently result in tissue avulsion, where portions of the cryptic lining are torn away along with the stone. This type of injury typically involves significant bleeding due to the rich vascular supply of the tonsillar parenchyma and the difficulty of achieving hemostasis in deep cryptic wounds.
Professional extraction procedures, while generally safer than self-removal attempts, also carry inherent bleeding risks that must be carefully managed through proper technique and patient selection. The use of inappropriate instruments, excessive force, or inadequate visualisation during stone removal can result in significant tissue trauma and bleeding complications. Additionally, the presence of underlying bleeding disorders, anticoagulant therapy, or severe chronic inflammation may contraindicate mechanical extraction approaches, necessitating alternative treatment strategies such as medical management or surgical intervention to address both the stones and associated bleeding risk.
Patient education regarding the risks of self-extraction represents a critical component of tonsillolith management, as many individuals attempt removal using dangerous techniques that significantly increase bleeding risk. Common mistakes include using sharp or rigid instruments, applying excessive force, or attempting removal in poorly visualised cryptic recesses where tissue damage is more likely. Healthcare providers must emphasise the importance of professional evaluation and treatment while providing patients with safe alternatives for symptom management until appropriate care can be obtained.
Differential diagnosis: tonsillar carcinoma versus tonsillolith bleeding
The differential diagnosis between bleeding caused by benign tonsilloliths and that associated with tonsillar malignancy represents one of the most
challenging aspects of tonsillar pathology evaluation, requiring careful consideration of multiple clinical and histological factors. While tonsilloliths represent a benign condition that may cause bleeding through mechanical and inflammatory mechanisms, tonsillar carcinoma presents as a potentially life-threatening malignancy that often manifests with similar hemorrhagic symptoms. The clinical overlap between these conditions necessitates systematic evaluation approaches that can reliably distinguish between benign calcified deposits and malignant transformation, particularly given the significant implications for patient management and prognosis.
The presentation patterns of bleeding in benign tonsillolith cases typically demonstrate specific characteristics that can aid in differential diagnosis. Tonsillolith-associated bleeding usually occurs in discrete episodes related to mechanical trauma, extraction attempts, or acute inflammatory exacerbations, with intervening periods of minimal or no bleeding. The bleeding tends to be superficial, originating from cryptic epithelium or superficial vascular structures, and responds well to conservative hemostatic measures. Additionally, the presence of visible calcified deposits within tonsillar crypts, characteristic halitosis, and history of recurrent stone formation provide supportive evidence for a benign etiology.
Conversely, bleeding associated with tonsillar carcinoma often presents with more concerning features that should prompt immediate oncological evaluation. Malignancy-related bleeding tends to be more persistent and progressive, often accompanied by other suspicious symptoms such as unilateral tonsillar enlargement, cervical lymphadenopathy, unexplained weight loss, or referred otalgia. The bleeding may appear more extensive and deep-seated, potentially involving larger vessels within the tonsillar parenchyma, and may be accompanied by tissue friability and irregular surface textures that differ markedly from the smooth, calcified appearance of benign tonsilloliths.
The distinction between benign tonsillolith bleeding and malignancy-associated hemorrhage requires careful evaluation of bleeding patterns, associated symptoms, and tissue characteristics, as misdiagnosis can have profound implications for patient outcomes and survival.
Advanced imaging studies play an increasingly important role in distinguishing between these conditions, particularly when clinical examination findings remain ambiguous. Computed tomography with contrast can reveal the characteristic high-density, calcified appearance of tonsilloliths while simultaneously identifying any suspicious soft tissue masses or abnormal enhancement patterns suggestive of malignancy. Magnetic resonance imaging provides superior soft tissue characterization that can help identify infiltrative growth patterns, perineural spread, or deep tissue invasion that would be inconsistent with benign tonsillolith formation. However, the definitive diagnosis often requires histopathological examination through targeted biopsy of suspicious areas, particularly when imaging findings remain inconclusive or when clinical suspicion for malignancy persists despite apparently benign imaging characteristics.