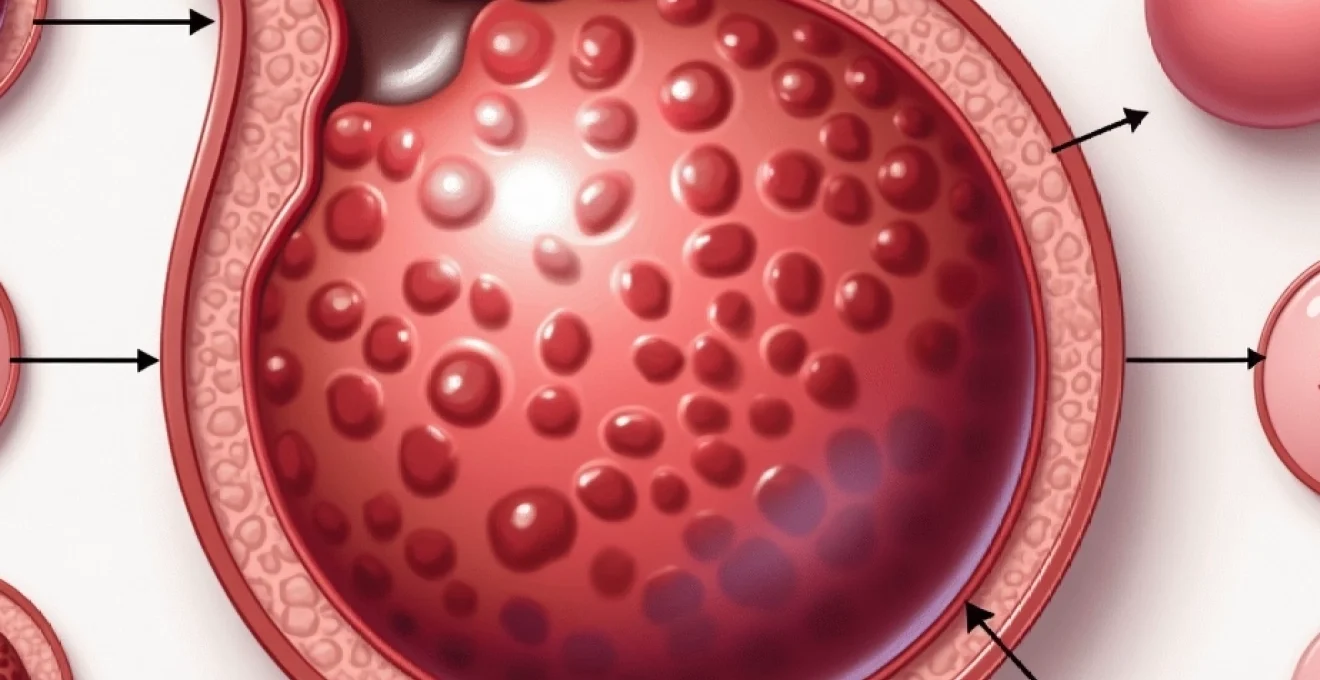
Blood blisters on the glans penis represent a concerning symptom that can cause significant anxiety for men experiencing this condition. These haemorrhagic lesions, characterised by localised collections of blood beneath the delicate skin of the penile head, can arise from numerous underlying causes ranging from benign traumatic injuries to more serious infectious or systemic conditions. The glans penis, with its rich vascular supply and sensitive epithelium, is particularly susceptible to various forms of trauma and pathological processes that can result in blood vessel rupture and subsequent blister formation.
Understanding the diverse aetiologies behind glans blood blisters is crucial for appropriate medical management and patient reassurance. While many cases resolve spontaneously without intervention, certain underlying conditions require prompt medical attention to prevent complications or address serious health concerns. The clinical presentation, associated symptoms, and patient history often provide valuable clues to distinguish between different causative factors and guide appropriate treatment strategies.
Traumatic blood blister formation on glans penis
Trauma remains the most common cause of blood blister development on the glans penis, with various mechanisms capable of damaging the delicate capillary networks beneath the surface epithelium. The glans contains numerous small blood vessels that are vulnerable to rupture when subjected to mechanical stress, compression, or sudden impact forces.
Friction-induced haematomas during sexual activity
Sexual activity represents a significant risk factor for traumatic blood blister formation on the glans penis. The repetitive friction and pressure associated with intercourse can cause microscopic tears in blood vessel walls, leading to localised haemorrhage and blister development. Inadequate lubrication particularly increases the risk of such injuries, as dry friction creates substantially more mechanical stress on the delicate glans tissue.
Vigorous or prolonged sexual activity can overwhelm the natural resilience of penile blood vessels, especially in cases where partners engage in forceful movements or unusual positions that place excessive strain on the penis. The resulting blood blisters typically appear within hours of the traumatic event and may be accompanied by mild to moderate pain, swelling, or discolouration of the surrounding tissue.
Mechanical trauma from masturbation techniques
Aggressive or inappropriate masturbation techniques frequently contribute to glans trauma and subsequent blood blister formation. Excessive force, inadequate lubrication, or the use of inappropriate objects during self-stimulation can cause significant mechanical stress to the penile tissues. Men who employ particularly vigorous techniques or engage in prolonged masturbation sessions are at higher risk of developing these haemorrhagic lesions.
The “death grip” syndrome, where individuals use excessive pressure during masturbation, can cause repeated microtrauma to glans blood vessels, potentially leading to chronic issues with blood blister formation. Additionally, the use of household objects or inappropriate devices as masturbation aids significantly increases the risk of severe trauma and complications beyond simple blood blisters.
Zipper entrapment and Clothing-Related injuries
Zipper entrapment injuries represent a particularly distressing cause of glans trauma that can result in blood blister formation. These accidents typically occur when penile skin becomes caught in clothing zippers, causing compression and shearing forces that damage blood vessels. The combination of pressure and attempted removal often exacerbates the initial injury, leading to more extensive tissue damage.
Tight clothing, particularly underwear or pants that compress the genital area, can also contribute to blood blister development through chronic pressure and friction. Athletes and individuals who wear restrictive clothing for extended periods may experience repeated minor trauma that eventually manifests as blood blisters on the glans or other penile areas.
Sports-related genital trauma and blood vessel rupture
Contact sports and high-impact activities pose significant risks for genital trauma that can result in glans blood blisters. Direct blows to the groin area, falls onto hard surfaces, or collision injuries can cause immediate blood vessel rupture and haematoma formation. Cycling, martial arts, and contact sports like rugby or American football present particular risks for such injuries.
The use of protective equipment can significantly reduce the risk of sports-related genital trauma, yet many athletes fail to utilise appropriate protection consistently. When trauma does occur, the rich vascular supply of the glans can lead to dramatic-appearing blood blisters that may seem more serious than they actually are, though proper medical evaluation remains essential.
Infectious aetiologies causing glans haemorrhagic lesions
Various infectious agents can cause inflammatory responses in the glans penis that result in blood blister formation or haemorrhagic lesions that may be mistaken for traumatic blood blisters. These infectious causes often present with additional symptoms that help distinguish them from purely traumatic aetiologies.
Herpes simplex virus type 1 and 2 vesicular eruptions
Herpes simplex virus infections represent one of the most common infectious causes of penile lesions that may appear similar to blood blisters. Both HSV-1 and HSV-2 can cause vesicular eruptions on the glans penis that initially present as clear or slightly cloudy fluid-filled blisters before potentially becoming haemorrhagic due to secondary trauma or inflammation.
The characteristic progression of herpes lesions from vesicles to ulcers, combined with associated symptoms such as burning, tingling, or prodromal sensations, helps distinguish these viral infections from traumatic blood blisters. Primary herpes infections often present with more severe symptoms, including systemic manifestations like fever and malaise, while recurrent episodes typically show milder local symptoms.
Herpes-related lesions may become haemorrhagic when patients scratch or inadvertently traumatise the vesicles, leading to secondary bleeding into the blister cavity. This can create confusion in diagnosis, particularly when patients present after the initial vesicular stage has passed and only haemorrhagic lesions remain visible.
Human Papillomavirus-Induced vascular proliferation
Human papillomavirus infections can occasionally cause vascular proliferation and abnormal blood vessel formation in genital tissues, potentially leading to lesions that may resemble blood blisters. While HPV more commonly causes typical wart-like growths, certain viral strains can induce significant vascular changes that result in haemorrhagic lesions.
Condylomata acuminata associated with HPV infection sometimes develop secondary haemorrhage due to trauma or inflammation, creating blood-filled lesions that may be confused with primary blood blisters. The presence of other characteristic HPV lesions, such as cauliflower-like growths or flat warts, often helps establish the correct diagnosis.
Candida albicans inflammatory response and capillary damage
Candidal balanitis can cause significant inflammatory responses in the glans penis that may result in capillary damage and subsequent blood blister formation. The inflammatory mediators released during fungal infections can compromise blood vessel integrity, making them more susceptible to rupture and haemorrhage formation.
Severe candidal infections may cause erosive changes in the glans epithelium that can become secondarily infected or traumatised, leading to haemorrhagic lesions. Immunocompromised patients are particularly susceptible to aggressive candidal infections that may present with unusual manifestations, including blood-filled lesions that might be mistaken for traumatic blood blisters.
Bacterial balanitis with secondary haemorrhagic complications
Bacterial infections of the glans penis can cause severe inflammatory responses that compromise local blood vessel integrity and lead to haemorrhagic complications. Staphylococcal and streptococcal infections are particularly associated with aggressive inflammatory responses that can result in blood vessel damage and subsequent blister formation.
The presence of purulent discharge, significant erythema, and systemic symptoms such as fever often distinguishes bacterial balanitis from other causes of glans blood blisters. Diabetic patients show increased susceptibility to bacterial infections and may develop more severe haemorrhagic complications due to compromised immune responses and poor wound healing capabilities.
Early recognition and appropriate antibiotic treatment of bacterial balanitis are crucial to prevent progression to more serious complications, including necrotising infections that can threaten penile viability.
Dermatological conditions manifesting as glans blood blisters
Several dermatological conditions can affect the genital area and present with lesions that may appear similar to blood blisters on the glans penis. These conditions often have characteristic patterns of distribution and associated symptoms that help distinguish them from purely traumatic or infectious causes of blood blister formation.
Bullous pemphigoid, though rare in genital locations, can occasionally affect the glans penis and cause blood-filled blisters due to the autoimmune destruction of basement membrane components. This condition typically affects elderly individuals and may present with widespread bullous lesions on other body areas, providing important diagnostic clues. The blisters in bullous pemphigoid are often tense and may persist for extended periods without rupturing, unlike traumatic blood blisters that typically resolve more quickly.
Stevens-Johnson syndrome and toxic epidermal necrolysis represent severe mucocutaneous reactions that can involve genital tissues and cause haemorrhagic bullae on the glans penis. These conditions are often triggered by medications or infections and present with characteristic widespread mucosal involvement, including oral and ocular manifestations. The presence of fever, malaise, and progression to epidermal detachment distinguishes these serious conditions from isolated glans blood blisters of other aetiologies.
Fixed drug eruptions can occasionally affect the glans penis and present as bullous lesions that may become haemorrhagic. These lesions characteristically recur in the same location with repeated exposure to the offending medication and often leave residual hyperpigmentation. Common causative medications include antibiotics, nonsteroidal anti-inflammatory drugs, and antimalarials, though virtually any medication can potentially cause fixed drug eruptions.
Behcet’s disease, a chronic multisystem inflammatory condition, can cause recurrent genital ulcerations that may initially present as blood-filled blisters before progressing to painful ulcers. The diagnosis is supported by the presence of characteristic oral aphthous ulcers, ocular involvement, and other systemic manifestations. The recurrent nature of Behcet’s lesions and their tendency to heal with scarring helps distinguish them from other causes of glans blood blisters.
Vascular malformations and congenital blood vessel abnormalities
Congenital vascular malformations affecting the glans penis can predispose individuals to blood blister formation through abnormal blood vessel structure and function. These conditions may not become apparent until adulthood when trauma or other triggering factors cause bleeding into malformed vascular structures, creating blood-filled lesions that may be mistaken for acquired blood blisters.
Arteriovenous malformations, though rare in genital locations, can cause localised areas of abnormal blood flow and vessel fragility that make the affected tissue susceptible to haemorrhage formation. These malformations may present as chronic, recurrent blood-filled lesions that appear spontaneously or after minimal trauma. Imaging studies, particularly colour Doppler ultrasonography , can help identify abnormal vascular flow patterns and confirm the diagnosis of underlying vascular malformations.
Capillary malformations, previously known as port-wine stains, can occasionally affect genital areas and may become more prominent or symptomatic with age due to progressive vascular ectasia. While these lesions are typically present from birth, they may not become clinically significant until later in life when hormonal changes or repeated trauma cause them to bleed or form blood-filled cysts.
Venous malformations can cause localised areas of abnormal venous drainage that result in chronic congestion and increased susceptibility to haemorrhage formation. These lesions may present as soft, compressible masses that can become painful and may develop secondary thrombosis or bleeding. The characteristic blue discolouration and softness of venous malformations help distinguish them from other vascular lesions affecting the glans penis.
Comprehensive evaluation of recurrent or unusual blood blisters on the glans should include consideration of underlying vascular malformations, particularly when lesions appear spontaneously or with minimal trauma.
Pharmacological causes and Drug-Induced haemorrhagic responses
Various medications can predispose patients to blood blister formation on the glans penis through different mechanisms, including altered coagulation function, increased vessel fragility, or direct toxic effects on vascular endothelium. Understanding these pharmacological relationships is crucial for proper diagnosis and management of drug-related glans haemorrhagic lesions.
Anticoagulant medications, including warfarin, heparin, and direct oral anticoagulants, significantly increase bleeding risk and can cause spontaneous haemorrhage into tissues with minimal trauma. Patients taking these medications may develop blood blisters on the glans penis after activities that would not typically cause such lesions in individuals with normal coagulation function. The risk is particularly elevated when anticoagulation levels are supratherapeutic or when patients concurrently use other medications that affect bleeding risk.
Antiplatelet agents, such as aspirin, clopidogrel, and other platelet aggregation inhibitors, can impair normal haemostatic responses and lead to prolonged bleeding from minor trauma. These medications may cause blood blisters to form more easily and persist longer than would be expected in patients with normal platelet function. The combination of multiple antiplatelet agents or concurrent use with anticoagulants significantly amplifies bleeding risks.
Certain antimicrobial agents, particularly those known to cause thrombocytopenia or platelet dysfunction, can predispose patients to haemorrhagic complications including glans blood blisters. Quinolones, sulfonamides, and vancomycin are among the antibiotics most commonly associated with platelet-related bleeding complications. The temporal relationship between medication initiation and symptom onset often provides crucial diagnostic information.
Chemotherapeutic agents can cause severe thrombocytopenia and coagulopathy that predispose patients to spontaneous bleeding and blood blister formation. Cancer patients receiving treatment may develop glans blood blisters as part of generalised bleeding tendencies and require careful monitoring of haematological parameters. The use of supportive care measures, including platelet transfusions, may be necessary in severe cases.
Systemic medical conditions contributing to penile blood blister development
Various systemic medical conditions can predispose patients to blood blister formation on the glans penis through mechanisms including altered coagulation function, compromised vascular integrity, or increased susceptibility to trauma-related bleeding. Recognition of these underlying conditions is essential for comprehensive patient care and prevention of recurrent episodes.
Haematological disorders, including thrombocytopenia, platelet function disorders, and coagulation factor deficiencies, can manifest with spontaneous bleeding or easy bruising that may include blood blister formation on the glans penis. Von Willebrand disease , the most common inherited bleeding disorder, can cause excessive bleeding from minor trauma and may present with unusual bleeding patterns including genital haemorrhagic lesions. Comprehensive haematological evaluation is warranted when blood blisters occur with minimal or no apparent trauma.
Diabetes mellitus contributes to blood blister formation through multiple mechanisms, including compromised wound healing, increased infection susceptibility, and diabetic microangiopathy that affects small blood vessels throughout the body. Diabetic patients may experience more frequent and severe blood blisters on the glans penis, particularly in the setting of poor glycaemic control or diabetic complications affecting vascular function.
Chronic kidney disease can cause bleeding complications through multiple mechanisms, including platelet dysfunction associated with uraemia, altered medication metabolism affecting anticoagulant drugs, and chronic inflammation that compromises vascular integrity. Patients with advanced chronic kidney disease may develop spontaneous bleeding tendencies that can manifest as blood blisters in various locations, including the glans penis.
Autoimmune conditions, particularly systemic lupus erythematosus and vasculitic disorders, can affect small blood vessels and cause increased bleeding tendencies that may result in glans blood blister formation. Antiphospholipid syndrome presents a paradoxical situation where patients may experience both thrombotic and bleeding complications, depending on the specific antibodies present
and treatment-resistant thrombocytopenia that can complicate bleeding management.
Liver disease significantly affects coagulation function through impaired synthesis of clotting factors, altered platelet production and function, and portal hypertension that can affect systemic bleeding risks. Patients with chronic liver disease may experience prolonged bleeding from minor trauma and increased susceptibility to blood blister formation throughout the body, including the genital area. The combination of decreased albumin synthesis and altered vascular permeability in liver disease can also contribute to tissue fragility and bleeding complications.
Hypertension, particularly when poorly controlled, can contribute to vascular fragility and increased bleeding risk that may manifest as spontaneous blood blister formation. The chronic pressure effects on small blood vessels can compromise their structural integrity, making them more susceptible to rupture with minimal trauma. Antihypertensive medications, particularly those affecting platelet function or coagulation, can further compound bleeding risks in hypertensive patients.
Comprehensive medical evaluation is essential when blood blisters on the glans penis occur repeatedly or in association with bleeding in other locations, as this may indicate underlying systemic disease requiring specific treatment.
Age-related changes in vascular structure and function can predispose elderly patients to blood blister formation through decreased vessel elasticity, compromised endothelial function, and reduced tissue healing capacity. Elderly men may experience more frequent and severe blood blisters from trauma that would cause minimal injury in younger individuals. The combination of age-related vascular changes with common comorbidities and medications further increases bleeding risks in this population.
Nutritional deficiencies, particularly those affecting vitamin C, vitamin K, or folate levels, can compromise vascular integrity and coagulation function, leading to increased bleeding tendencies. Scurvy, though rare in developed countries, can cause significant capillary fragility and bleeding complications when it occurs. Patients with malabsorption syndromes or restrictive diets may develop nutritional deficiencies that contribute to bleeding disorders and blood blister formation.