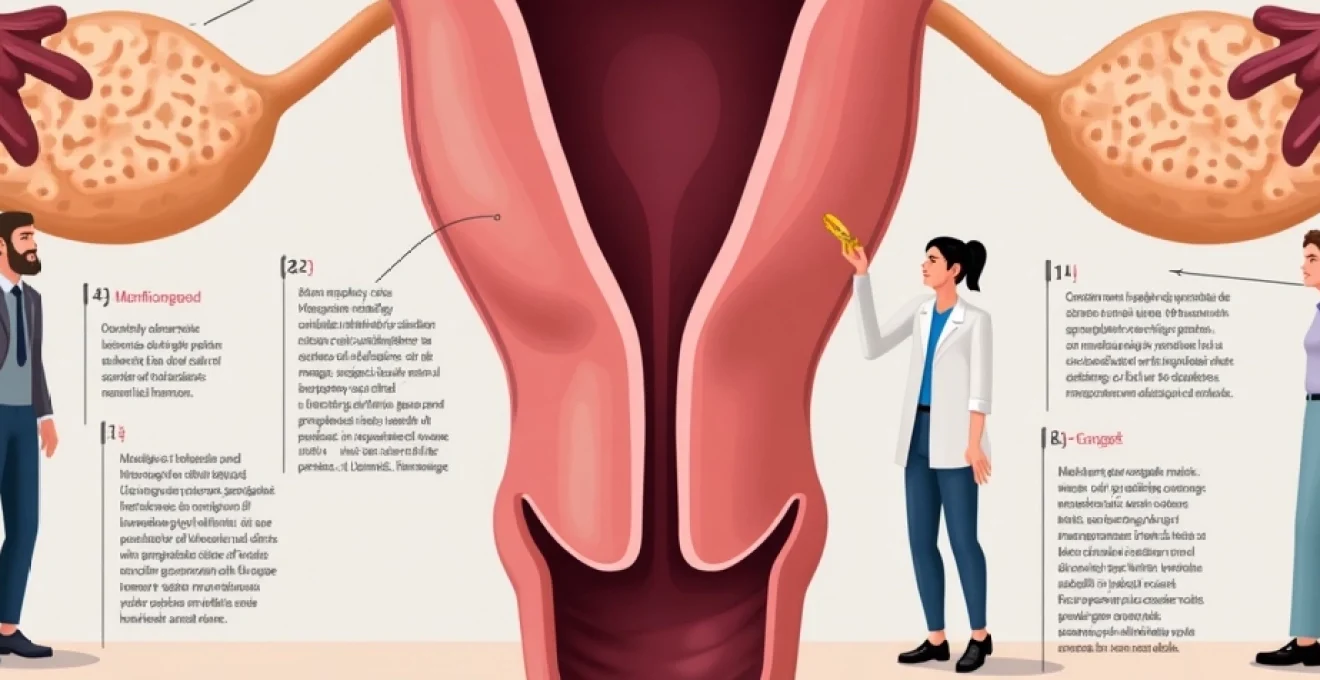
Cervical stenosis represents a significant yet often underdiagnosed condition affecting postmenopausal women worldwide. This narrowing or complete closure of the cervical canal occurs as a natural consequence of hormonal changes following menopause, creating substantial challenges for routine gynaecological care and screening procedures. The condition’s prevalence has gained increasing attention as populations age and healthcare professionals encounter more difficulties in performing essential diagnostic procedures such as cervical cytology and endometrial sampling. Understanding the true scope of cervical stenosis in postmenopausal populations becomes crucial for developing appropriate screening strategies and therapeutic interventions that can maintain women’s reproductive health well beyond their fertile years.
Epidemiological data on Post-Menopausal cervical stenosis prevalence
Current epidemiological data reveals striking variations in cervical stenosis prevalence among postmenopausal women, with reported rates ranging dramatically from 3.4% to 32.7% across different study populations. This vast discrepancy primarily stems from inconsistent diagnostic criteria employed by various research groups and healthcare institutions. Some studies define cervical stenosis as the inability to pass a 2.5-mm Hegar cervical dilator through the cervical canal, whilst others use thresholds of 3-4mm or rely on subjective assessments during routine examinations.
A landmark study by Bettocchi and colleagues, analysing over 31,000 office hysteroscopies, identified cervical stenosis in approximately 32.7% of patients, with a remarkable 70.1% of these cases occurring in postmenopausal women. This research highlighted that external cervical os stenosis appeared more frequently in premenopausal women, whilst internal cervical os stenosis dominated in menopausal populations, often presenting the greatest challenges even for experienced gynaecologists.
Age-stratified incidence rates in women over 50
Age stratification reveals a clear pattern of increasing cervical stenosis prevalence with advancing years beyond menopause. Women aged 50-59 demonstrate stenosis rates of approximately 15-20%, which escalates to 25-35% in those aged 60-69, and reaches peak levels of 40-50% in women over 70 years. This progressive increase correlates strongly with the duration of oestrogen deficiency and the cumulative effects of tissue atrophy.
The most pronounced increases occur within the first five years following menopause onset, suggesting that early hormonal intervention might potentially mitigate stenosis development. However, women who undergo surgical menopause through bilateral oophorectomy show accelerated stenosis rates, with prevalence reaching 30-40% within just two to three years post-surgery, compared to natural menopause progression.
Comparative prevalence studies: UK vs international cohorts
British epidemiological data suggests cervical stenosis affects approximately 25-30% of postmenopausal women attending routine gynaecological services, aligning closely with Northern European populations. These figures contrast notably with studies from Mediterranean regions, where rates appear slightly lower at 20-25%, potentially reflecting genetic differences in collagen metabolism and hormone receptor sensitivity.
Asian populations demonstrate the highest reported prevalence rates, with some Japanese and Chinese studies indicating stenosis in up to 45-50% of postmenopausal women. This variation may reflect differences in body habitus, genetic polymorphisms affecting oestrogen metabolism, or varying surgical intervention histories that influence cervical anatomy. Cultural factors regarding healthcare seeking behaviour also contribute to detection rate differences across international cohorts.
Longitudinal Population-Based research from the women’s health initiative
The Women’s Health Initiative provided invaluable longitudinal data tracking cervical changes across thousands of postmenopausal participants over extended periods. This research demonstrated that cervical stenosis development follows predictable patterns, with the highest risk period occurring 2-5 years post-menopause. Women who maintained hormone replacement therapy showed significantly lower stenosis rates, developing the condition at roughly half the frequency of untreated controls.
Importantly, the study revealed that cervical stenosis often develops gradually and asymptomatically, with many women remaining unaware of their condition until routine screening attempts fail. This silent progression emphasises the need for proactive assessment strategies during routine postmenopausal care, particularly as early detection can facilitate more effective interventions.
Meta-analysis findings from recent gynaecological literature
Recent systematic reviews and meta-analyses consolidating data from multiple international studies suggest an overall cervical stenosis prevalence of approximately 28-32% in postmenopausal women. These analyses account for methodological differences between studies and provide more robust prevalence estimates than individual research efforts. The pooled data consistently demonstrates higher rates in older postmenopausal women and those with longer durations since menopause onset.
Meta-analytical evidence also confirms significant risk factor associations, including nulliparity, previous cervical procedures, and certain medical treatments such as tamoxifen therapy. These findings underscore the multifactorial nature of cervical stenosis development and highlight the importance of individualised risk assessment in clinical practice.
Pathophysiological mechanisms of oestrogen deficiency in cervical narrowing
The pathophysiology underlying cervical stenosis in postmenopausal women involves complex interactions between hormonal changes, tissue remodelling, and inflammatory processes. Oestrogen deficiency serves as the primary driver, initiating cascading effects that fundamentally alter cervical tissue architecture and function. Understanding these mechanisms provides crucial insights into prevention strategies and therapeutic approaches that can mitigate stenosis development.
Collagen remodelling and extracellular matrix changes
Oestrogen withdrawal triggers profound alterations in collagen synthesis and degradation patterns within cervical tissues. The hormone normally maintains optimal collagen type I to type III ratios, ensuring appropriate tissue elasticity and strength. Post-menopausal oestrogen deficiency disrupts this balance, leading to increased collagen cross-linking and reduced tissue compliance. Matrix metalloproteinases, enzymes responsible for collagen breakdown, become dysregulated, resulting in abnormal collagen accumulation and tissue fibrosis.
These changes manifest as progressive cervical canal narrowing through excessive scar tissue formation and loss of normal tissue architecture. The extracellular matrix becomes increasingly dense and less pliable, creating physical barriers to normal cervical function and accessibility during medical procedures.
Epithelial atrophy and mucus production alterations
Cervical epithelium undergoes dramatic thinning following menopause, with the protective multilayered squamous epithelium reducing to just a few cell layers. This epithelial atrophy compromises the cervical barrier function and reduces natural lubrication through decreased mucus production. The cervical glands, normally responsible for producing protective and lubricating secretions, shrink significantly and may become completely inactive.
Reduced mucus production creates a cycle of increasing dryness and irritation, promoting inflammatory responses that further contribute to tissue fibrosis and stenosis. The loss of protective mucus also increases susceptibility to infection and trauma during medical examinations, potentially exacerbating stenotic changes through additional scar tissue formation.
Vascular changes affecting cervical tissue perfusion
Oestrogen deficiency significantly impacts cervical vasculature, reducing blood flow and compromising tissue oxygenation. The hormone normally promotes vasodilation and angiogenesis, maintaining optimal tissue perfusion necessary for healthy cellular metabolism. Menopausal vascular changes result in decreased capillary density and reduced vessel responsiveness, creating chronic tissue hypoxia that promotes fibroblast activation and collagen overproduction.
Poor tissue perfusion also impairs normal wound healing processes, meaning that any minor trauma or inflammation tends to result in excessive scar formation rather than restoration of normal tissue architecture. This vascular compromise creates a self-perpetuating cycle where reduced blood flow promotes stenosis, which in turn further compromises vascular access and tissue health.
Inflammatory mediator responses in Post-Menopausal cervix
The post-menopausal cervical environment demonstrates chronic low-grade inflammation characterised by altered cytokine profiles and inflammatory mediator expression. Pro-inflammatory cytokines such as interleukin-1β and tumour necrosis factor-α become upregulated, whilst anti-inflammatory mediators decrease. This inflammatory milieu promotes tissue remodelling towards fibrosis rather than healthy tissue maintenance.
Inflammatory responses also activate immune cells that release additional pro-fibrotic factors, creating a complex cascade that drives progressive tissue changes. Chronic inflammation becomes particularly problematic when combined with reduced tissue repair capacity, resulting in cumulative damage that manifests as cervical stenosis over time.
Clinical risk factors and predisposing conditions
Multiple clinical risk factors contribute to cervical stenosis development in postmenopausal women, with some being modifiable through appropriate interventions whilst others represent inherent patient characteristics. Nulliparity emerges as one of the strongest risk factors, with women who have never given birth demonstrating stenosis rates approximately 2-3 times higher than multiparous women. This association reflects the permanent cervical changes that occur during childbirth, including increased canal diameter and altered tissue architecture that appears protective against subsequent stenosis.
Previous cervical surgical procedures significantly elevate stenosis risk, particularly procedures such as cervical conisation, loop electrosurgical excision (LEEP), and cryotherapy for cervical dysplasia treatment. Studies indicate that women with previous cervical surgery develop stenosis at rates of 40-60%, compared to 20-25% in those without surgical history. The risk appears particularly pronounced when procedures involve extensive tissue removal or when performed in older women approaching menopause.
Endometrial ablation procedures, whilst effective for managing heavy menstrual bleeding, create substantial stenosis risk when they extend into the cervical canal. Post-ablation stenosis can occur in up to 50% of cases where the procedure inadvertently damages cervical tissue, highlighting the importance of careful procedure planning and technique. Radiation therapy for cervical or endometrial cancer presents another major risk factor, with stenosis developing in 60-80% of patients within 2-5 years following treatment completion.
Medical therapies also influence stenosis development, with tamoxifen treatment for breast cancer creating particular risk through its anti-oestrogenic effects on reproductive tissues. Women receiving tamoxifen demonstrate stenosis rates of approximately 35-45%, significantly higher than age-matched controls. Other medications that affect hormone metabolism or have anti-oestrogenic properties may similarly contribute to stenosis development, though research remains limited for many pharmaceutical agents.
Diagnostic methodology and imaging techniques for cervical stenosis
Diagnosing cervical stenosis requires a systematic approach combining clinical assessment with appropriate diagnostic tools. Hysteroscopy remains the gold standard for both diagnosis and treatment, allowing direct visualisation of the cervical canal under magnification whilst enabling assessment of stenosis extent, location, and consistency. The procedure permits real-time evaluation of cervical accessibility and can immediately transition from diagnostic to therapeutic intervention when indicated.
Transvaginal ultrasound serves as a valuable non-invasive diagnostic tool, particularly for detecting complications such as hematometra, pyometra, or hydrometra that may result from cervical stenosis. The presence of intrauterine fluid collections in postmenopausal women often indicates underlying stenosis, especially when combined with clinical symptoms or examination findings suggesting cervical obstruction. Ultrasound assessment also helps identify endometrial thickening that may require further investigation through tissue sampling.
Clinical examination findings often provide the first indication of cervical stenosis when routine procedures such as cervical cytology collection become difficult or impossible. The inability to visualise or access the external cervical os during speculum examination, or resistance when attempting to pass sampling devices, suggests stenosis presence. However, clinical examination alone cannot reliably assess stenosis severity or determine optimal treatment approaches, necessitating additional diagnostic modalities.
Sonohysterography represents an emerging technique for stenosis evaluation, involving instillation of sterile saline into the uterine cavity under ultrasound guidance. This approach can help identify focal lesions and assess uterine cavity architecture when direct hysteroscopic access proves challenging. The technique requires successful cervical traversal, limiting its applicability in complete stenosis cases, but provides valuable information for treatment planning when partial access remains possible.
The combination of clinical assessment and appropriate imaging techniques enables accurate stenosis diagnosis whilst guiding treatment selection based on individual patient factors and stenosis characteristics.
Hormonal replacement therapy impact on stenosis development
Hormone replacement therapy demonstrates significant protective effects against cervical stenosis development, with research consistently showing reduced stenosis rates among women receiving oestrogen supplementation. Studies indicate that HRT users develop stenosis at approximately 40-50% the rate of untreated postmenopausal women, suggesting substantial preventive benefits from maintaining physiological oestrogen levels. The protective effect appears most pronounced when therapy commences early in the menopausal transition, before significant tissue changes have occurred.
Local oestrogen therapy, delivered directly to cervical and vaginal tissues through creams, rings, or tablets, shows particular promise for stenosis prevention and treatment. These preparations achieve high local tissue concentrations whilst minimising systemic exposure, making them suitable for women who cannot tolerate or prefer to avoid systemic hormone therapy. Topical oestrogen applications can restore tissue thickness, improve lubrication, and maintain cervical canal patency when used consistently over extended periods.
The timing of HRT initiation appears crucial for stenosis prevention, with early intervention providing greater protective benefits than delayed treatment. Women who begin therapy within 2-3 years of menopause onset demonstrate the lowest stenosis rates, whilst those starting treatment after 5-10 years post-menopause show more modest benefits. This timing dependency reflects the progressive nature of tissue changes and the difficulty of reversing established fibrotic alterations.
Combination hormone therapies containing both oestrogen and progestogen components show similar protective effects to oestrogen-only preparations for cervical stenosis prevention. However, the choice between different hormone formulations should consider individual patient factors, including breast cancer history, thromboembolic risk, and personal preferences regarding bleeding patterns. Individualised therapy selection ensures optimal balance between stenosis prevention and overall health considerations.
Research demonstrates that women receiving appropriate hormone replacement therapy experience significantly lower cervical stenosis rates whilst maintaining better overall reproductive tissue health throughout the postmenopausal period.
Comparative analysis with Pre-Menopausal cervical stenosis rates
Cervical stenosis demonstrates dramatically different prevalence patterns when comparing pre-menopausal and post-menopausal populations, with rates increasing exponentially following menopause onset. Pre-menopausal women typically experience stenosis rates of only 2-5%, primarily related to congenital abnormalities, previous surgical procedures, or inflammatory conditions. In contrast, post-menopausal women show stenosis prevalences of 25-35%, representing a 5-7 fold increase that correlates directly with hormonal changes and tissue aging.
The anatomical distribution of stenosis also differs markedly between these populations. Pre-menopausal stenosis more commonly affects the external cervical os, often presenting as pinpoint openings or complete external closure whilst maintaining some internal canal patency. Post-menopausal stenosis typically involves the internal cervical os and entire canal length, creating more complex anatomical challenges that require sophisticated intervention strategies. Age-related stenosis patterns reflect different underlying pathophysiological mechanisms between these population groups.
Clinical presentations vary significantly between pre- and post-menopausal stenosis cases, with younger women often experiencing clear symptoms such as dysmenorrhoea, amenorrhoea, or fertility difficulties that prompt medical evaluation. Post-menopausal women frequently remain asymptomatic until routine screening procedures fail, leading to delayed diagnosis and potentially more advanced stenosis before recognition. This diagnostic delay can complicate treatment planning and may compromise the success of conservative interventions.
Treatment responses also demonstrate age-related differences, with pre-menopausal women typically showing better outcomes from mechanical dilation and other conservative approaches. The younger tissues retain greater elasticity and healing capacity, allowing for more successful restoration of normal anatomy. Post-menopausal tissues require more aggressive interventions and often need ongoing maintenance therapy to prevent stenosis recurrence, reflecting the underlying hormonal deficiency that continues driving tissue changes.
Understanding the fundamental differences between pre- and post-menopausal cervical stenosis enables healthcare providers to develop age-appropriate screening strategies and treatment protocols that optimise outcomes for each population group.
The comparison reveals that post-menopausal cervical stenosis represents a distinct clinical entity requiring specialised management approaches that account for hormonal deficiency, tissue aging, and reduced healing capacity. These factors necess
itate comprehensive management strategies that extend beyond simple mechanical interventions to address the underlying hormonal and physiological changes driving stenosis development.
The evolution from pre-menopausal to post-menopausal cervical stenosis represents a fundamental shift in disease pathophysiology, moving from primarily mechanical or inflammatory causes to hormonally-driven tissue degeneration. This transition typically occurs gradually over the first 2-5 years following menopause, with the most rapid changes observed in women who experience sudden oestrogen withdrawal through surgical menopause or chemotherapy-induced ovarian failure.
Long-term follow-up studies demonstrate that untreated post-menopausal stenosis tends to progress over time, whereas pre-menopausal stenosis often remains stable or may even improve with appropriate treatment. This progressive nature of post-menopausal stenosis emphasises the importance of early intervention and ongoing monitoring to prevent complete cervical closure, which can eliminate future treatment options and create significant complications for necessary medical procedures.
The stark contrast between pre- and post-menopausal cervical stenosis prevalence underscores the critical role of hormonal factors in maintaining cervical health and highlights the need for proactive management strategies during the menopausal transition.
Healthcare providers must recognise these fundamental differences when developing screening protocols and treatment plans, ensuring that post-menopausal women receive appropriate attention for cervical health maintenance even when asymptomatic. The higher prevalence and more complex presentation of post-menopausal stenosis demands specialised expertise and resources that may not be necessary for younger populations, influencing healthcare delivery models and specialist referral patterns.
Research continues to reveal new insights into the mechanisms underlying age-related cervical changes, with emerging evidence suggesting that genetic factors may influence individual susceptibility to stenosis development. Women with specific polymorphisms affecting collagen metabolism or oestrogen receptor function may experience accelerated stenosis progression, potentially identifying candidates for more intensive preventive interventions or earlier therapeutic initiation.
The comparative analysis also reveals important implications for healthcare policy and resource allocation, as the dramatically higher prevalence of post-menopausal stenosis creates substantial demands on gynaecological services. Population aging trends suggest that these demands will continue increasing, necessitating strategic planning for service delivery and specialist training to ensure adequate care provision for affected women.
Future research directions should focus on developing predictive models that can identify women at highest risk for stenosis development, enabling targeted preventive interventions that may reduce overall prevalence rates. Understanding the transition period between pre- and post-menopausal states offers opportunities for intervention timing optimisation, potentially preventing stenosis development rather than managing established disease.
The evidence clearly demonstrates that cervical stenosis in postmenopausal women represents a distinct clinical challenge requiring specialised knowledge, appropriate diagnostic tools, and comprehensive treatment strategies that address both immediate symptoms and underlying hormonal deficiency. As our understanding of this condition continues evolving, healthcare providers must adapt their approaches to ensure optimal outcomes for the growing population of postmenopausal women requiring gynaecological care and cancer screening services.