Muscle indentations in the thigh can present as concerning visible or palpable depressions that develop in what should be smooth, continuous muscle contours. These anatomical changes often manifest as finger-length dents, grooves, or asymmetrical depressions that become particularly noticeable when wearing fitted clothing or during physical examination. While some individuals may dismiss these changes as cosmetic concerns, thigh muscle indentations frequently indicate underlying pathological processes affecting muscle integrity, neurological function, or vascular supply.
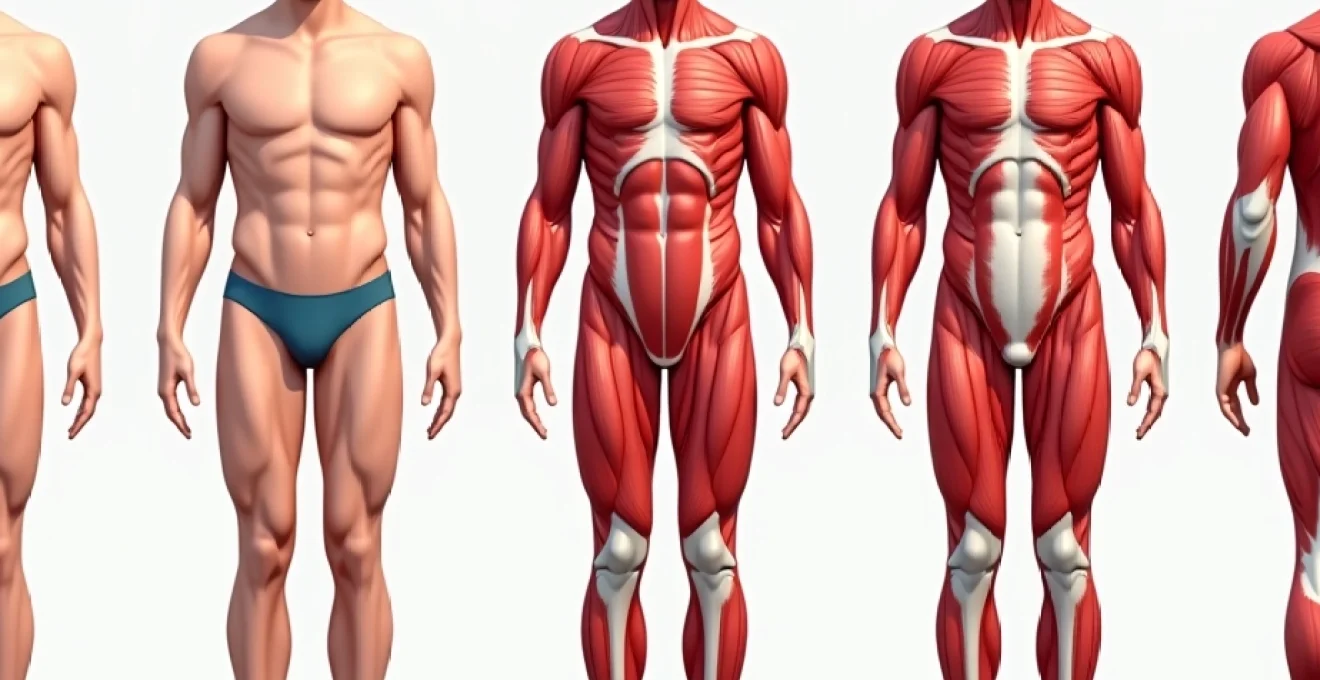
The quadriceps muscle group, comprising the vastus lateralis, vastus medialis, vastus intermedius, and rectus femoris, represents one of the most robust muscle complexes in the human body. When indentations develop within this muscular architecture, the underlying mechanisms can range from benign occupational hazards to serious neuromuscular disorders requiring immediate medical intervention. Understanding these diverse aetiologies becomes essential for healthcare professionals and individuals experiencing these changes alike.
Muscle atrophy and quadriceps wasting patterns
Muscle atrophy represents the most common underlying mechanism responsible for thigh muscle indentations, characterised by the progressive loss of muscle mass and subsequent volumetric reduction. This process typically develops gradually, creating visible depressions as surrounding healthy muscle tissue maintains its normal bulk whilst affected areas diminish. The quadriceps muscle group demonstrates particular vulnerability to atrophic changes due to its substantial metabolic demands and complex innervation patterns.
Vastus medialis oblique atrophy characteristics
The vastus medialis oblique (VMO) frequently exhibits selective atrophy patterns that create distinctive medial thigh indentations. This muscle component plays a crucial role in knee stabilisation and patellar tracking, making its preservation essential for optimal lower limb function. When VMO atrophy occurs, patients often notice a flattened appearance along the inner aspect of the thigh, particularly evident when the leg is extended or during weight-bearing activities.
Selective VMO wasting commonly develops following knee injuries, prolonged immobilisation, or reflex inhibition secondary to joint effusion. The resulting muscle indentation typically measures several centimetres in length and may be accompanied by functional deficits including knee instability and altered gait mechanics. Early recognition of VMO atrophy becomes paramount, as targeted rehabilitation can often restore muscle bulk and function when intervention begins promptly.
Rectus femoris muscle volume loss indicators
Rectus femoris atrophy manifests as longitudinal indentations along the anterior thigh, often creating a groove-like depression that extends from the hip towards the knee. This two-joint muscle crosses both the hip and knee, making it susceptible to injury and subsequent atrophic changes. The visual impact of rectus femoris volume loss can be particularly striking, as this muscle contributes significantly to the anterior thigh contour.
Athletes engaged in high-velocity activities such as sprinting or football demonstrate increased susceptibility to rectus femoris injuries and subsequent atrophy. The muscle’s role in hip flexion and knee extension means that functional deficits accompanying atrophic changes can significantly impact sporting performance and daily activities. Chronic rectus femoris atrophy may also indicate underlying hip pathology or lumbar spine dysfunction affecting muscle recruitment patterns.
Sarcopenia-related thigh muscle indentations
Age-related muscle loss, or sarcopenia, represents a progressive condition affecting muscle mass, strength, and function throughout the body. The quadriceps muscle group experiences disproportionate sarcopenic changes, with studies indicating muscle mass reductions of up to 40% between the ages of 20 and 80 years. This process creates characteristic indentations and contour changes that may initially appear subtle but progressively worsen without intervention.
Sarcopenic muscle indentations typically develop symmetrically and affect multiple muscle groups simultaneously. The process begins around the fourth decade of life, with an accelerated rate of muscle loss occurring after age 50. Nutritional factors, hormonal changes, and decreased physical activity contribute to sarcopenic progression, making early identification and intervention crucial for maintaining functional independence.
Disuse atrophy following prolonged immobilisation
Prolonged periods of reduced activity or complete immobilisation trigger rapid muscle atrophy through multiple physiological mechanisms. The quadriceps demonstrates particular susceptibility to disuse atrophy, with measurable muscle mass reductions occurring within days of immobilisation. This rapid onset distinguishes disuse atrophy from other atrophic processes and highlights the importance of early mobilisation in clinical settings.
Bed rest studies have demonstrated quadriceps muscle mass reductions of up to 20% within just two weeks of complete immobilisation. The resulting muscle indentations often appear asymmetrical if only one limb is affected, creating noticeable differences in thigh contour between legs. Recovery from disuse atrophy requires structured rehabilitation programmes incorporating progressive resistance training and functional movement patterns.
Neurological conditions causing thigh muscle indentation
Neurological disorders affecting the motor pathways supplying the quadriceps muscle group can produce characteristic patterns of muscle indentation through denervation-induced atrophy. These conditions disrupt the neural signals necessary for muscle contraction and maintenance, leading to progressive muscle wasting that manifests as visible depressions in the thigh contour. The pattern and distribution of muscle indentations often provide valuable diagnostic clues regarding the specific neurological pathology involved.
Femoral nerve palsy and quadriceps denervation
Femoral nerve palsy represents a devastating condition that can produce complete quadriceps denervation and subsequent massive muscle atrophy. The femoral nerve supplies all four components of the quadriceps muscle group, making its dysfunction particularly debilitating for lower limb function. Patients with femoral nerve palsy typically develop profound thigh muscle indentations within weeks of the initial injury, accompanied by severe functional deficits.
Common causes of femoral nerve palsy include diabetes mellitus, direct trauma, surgical complications, and compression from masses or haematomas. The resulting muscle indentations often appear dramatic, with entire muscle bellies appearing to collapse and create deep depressions in the thigh. Early electromyographic studies can help determine the extent of nerve damage and guide prognostic expectations for muscle recovery.
Lumbar radiculopathy L2-L4 muscle weakness patterns
Lumbar radiculopathy affecting the L2, L3, or L4 nerve roots can produce selective patterns of quadriceps weakness and subsequent muscle indentation. Each nerve root contributes to different aspects of quadriceps innervation, creating characteristic patterns of muscle involvement that can aid in diagnostic localisation. L3 radiculopathy commonly affects the vastus medialis, whilst L4 involvement typically impacts the vastus lateralis and rectus femoris.
The muscle indentations associated with lumbar radiculopathy often develop gradually over months, reflecting the chronic nature of nerve root compression. Patients may initially notice subtle asymmetries in thigh contour that progressively worsen without appropriate treatment. Magnetic resonance imaging of the lumbar spine typically reveals the underlying pathology, such as disc herniation or spinal stenosis, responsible for nerve root compromise.
Peripheral Neuropathy-Induced muscle wasting
Various forms of peripheral neuropathy can affect the motor nerves supplying the quadriceps, leading to muscle indentations through denervation atrophy. Diabetic neuropathy represents one of the most common causes, particularly affecting the femoral nerve and its branches. The resulting muscle wasting typically develops insidiously, with patients often unaware of the changes until significant muscle mass has been lost.
Inflammatory neuropathies, such as chronic inflammatory demyelinating polyneuropathy (CIDP), can also produce quadriceps muscle indentations through demyelination of motor nerve fibres. These conditions often present with fluctuating weakness patterns and may respond to immunosuppressive therapy if diagnosed promptly.
The key to successful management lies in early recognition of the underlying neuropathic process and initiation of appropriate disease-specific treatment.
Spinal cord injury motor unit loss
Spinal cord injuries affecting the lumbar segments can produce varying degrees of quadriceps muscle denervation depending on the level and completeness of the lesion. Incomplete spinal cord injuries may result in partial muscle preservation with selective indentations affecting specific muscle groups. Complete lesions typically produce profound muscle atrophy affecting the entire quadriceps complex.
The pattern of muscle indentation following spinal cord injury often correlates with the neurological level of injury and can provide insights into the extent of neural damage. Upper motor neuron lesions may initially preserve muscle bulk through spasticity, whilst lower motor neuron involvement results in rapid muscle atrophy and indentation formation. Functional electrical stimulation programmes have shown promise in maintaining muscle bulk and potentially reducing the severity of muscle indentations in appropriate candidates.
Vascular insufficiency and compartment syndrome effects
Vascular compromise affecting the thigh musculature can produce muscle indentations through ischaemic injury and subsequent fibrotic replacement of healthy muscle tissue. Chronic compartment syndrome represents a particularly relevant condition in athletic populations, where repeated episodes of elevated compartment pressure can lead to muscle damage and characteristic indentation patterns. The anterior thigh compartment, containing the quadriceps muscle group, demonstrates particular vulnerability to pressure-related ischaemic changes.
Acute compartment syndrome, whilst rare in the thigh, can produce devastating muscle necrosis when it occurs. The massive swelling associated with acute compartment syndrome initially obscures muscle contours, but subsequent resolution reveals characteristic indentations corresponding to areas of muscle death. Early recognition and surgical decompression represent the only effective treatments for preventing permanent muscle damage and indentation formation.
Chronic arterial insufficiency, particularly in elderly patients with peripheral vascular disease, can contribute to gradual muscle atrophy and indentation development. The reduced blood flow impairs muscle metabolism and protein synthesis, leading to progressive muscle wasting. Vascular assessment through ankle-brachial indices and duplex ultrasonography can help identify compromised arterial supply as a contributing factor to thigh muscle indentations.
Post-surgical complications and iatrogenic muscle damage
Surgical procedures involving the thigh or adjacent anatomical structures can inadvertently damage muscle tissue or its nerve supply, resulting in characteristic indentation patterns. The complexity of thigh anatomy, with its multiple muscle layers and neurovascular structures, makes surgical complications affecting muscle integrity a recognised risk across various procedures. Understanding these iatrogenic causes becomes essential for both preventing complications and managing their consequences when they occur.
Arthroscopic surgery quadriceps inhibition
Knee arthroscopy, despite its minimally invasive nature, frequently produces temporary quadriceps inhibition that can progress to muscle atrophy if not addressed promptly. The mechanisms include direct trauma from portal placement, joint effusion, and reflex inhibition secondary to intra-articular inflammation. Studies demonstrate measurable quadriceps atrophy within days of arthroscopic procedures, with some patients developing visible muscle indentations that persist for months.
The vastus medialis oblique demonstrates particular vulnerability to post-arthroscopic atrophy, often creating medial thigh indentations that become apparent during the early rehabilitation period. Accelerated rehabilitation protocols incorporating early quadriceps activation exercises have proven effective in minimising muscle atrophy and preventing permanent indentation formation. Cryotherapy and electrical stimulation represent additional interventions that can help maintain muscle bulk during the acute post-operative period.
Total knee replacement muscle trauma
Total knee replacement surgery involves significant soft tissue manipulation that can result in direct quadriceps muscle damage and subsequent indentation formation. The surgical approach requires extensive exposure of the knee joint, often involving quadriceps tendon manipulation or partial detachment. Post-operative immobilisation and pain-related muscle guarding further contribute to muscle atrophy and indentation development.
Research indicates that quadriceps muscle strength may remain diminished by 20-30% even years after total knee replacement, reflecting persistent structural changes in muscle architecture. The resulting muscle indentations often correlate with functional deficits and may impact patient satisfaction with surgical outcomes.
Aggressive pre-operative conditioning and post-operative rehabilitation represent the most effective strategies for minimising muscle atrophy and indentation formation following total knee replacement.
Liposuction-related fascial plane disruption
Cosmetic liposuction procedures targeting thigh fat deposits can inadvertently damage underlying fascial planes and muscle architecture, creating irregular indentations that may mimic muscle atrophy. Over-aggressive fat removal or poor surgical technique can disrupt the natural contours of the thigh, resulting in visible depressions that become apparent as post-operative swelling resolves.
The phenomenon of semicircular lipoatrophy, whilst typically associated with external pressure, can also occur following liposuction procedures through disruption of local fat architecture. These indentations often appear as linear or curved depressions that may persist indefinitely without corrective intervention. Careful patient selection and conservative fat removal techniques represent the primary preventive measures for avoiding these complications.
Inflammatory myopathies and autoimmune muscle disorders
Inflammatory muscle diseases represent a diverse group of conditions that can produce characteristic patterns of muscle atrophy and indentation through immune-mediated muscle destruction. These disorders typically affect multiple muscle groups but may demonstrate selective patterns that create distinctive indentation patterns in the thigh musculature. The inflammatory process damages muscle fibres directly whilst also disrupting the supporting connective tissue architecture.
Polymyositis and dermatomyositis represent the most common inflammatory myopathies affecting the quadriceps muscle group. These conditions typically produce symmetric muscle weakness and atrophy, creating bilateral thigh indentations that develop gradually over months. The inflammatory process can be visualised on magnetic resonance imaging as areas of increased signal intensity within affected muscles, corresponding to areas of active inflammation and subsequent atrophy.
Inclusion body myositis demonstrates a predilection for affecting the quadriceps muscle group, often creating asymmetric indentations that may initially suggest neurological pathology. This condition typically affects older adults and demonstrates a characteristic pattern of selective muscle involvement that includes the quadriceps, finger flexors, and ankle dorsiflexors. Muscle biopsy remains the gold standard for diagnosing inflammatory myopathies and can help distinguish between different subtypes based on characteristic histological features.
Systemic lupus erythematosus and other connective tissue disorders can produce muscle indentations through various mechanisms including direct muscle inflammation, steroid-induced myopathy, and vascular compromise. The multisystem nature of these conditions often provides additional clinical clues that aid in diagnosis, such as characteristic rashes, joint involvement, or organ dysfunction. Treatment typically involves immunosuppressive therapy, though the response varies considerably between different conditions and individual patients.
Diagnostic imaging protocols for thigh muscle indentation assessment
Comprehensive evaluation of thigh muscle indentations requires a systematic approach incorporating multiple imaging modalities to identify the underlying pathological process. Magnetic resonance imaging represents the gold standard for assessing muscle architecture, providing detailed visualisation of muscle bulk, signal characteristics, and surrounding anatomical structures. The protocol should include both T1-weighted and T2-weighted sequences to differentiate between acute inflammatory changes and chronic atrophic processes.
Ultrasound imaging offers a cost-effective and readily available alternative for assessing muscle bulk and architecture, particularly useful for monitoring changes over time or during rehabilitation. High-frequency transducers can visualise individual muscle fibres and detect subtle changes in muscle echogenicity that may indicate ongoing pathological processes. Real-time ultrasound assessment during muscle contraction can provide additional information about muscle function and recruitment patterns.
Computed tomography, whilst less commonly used for muscle assessment, provides excellent visualisation of muscle cross-sectional area and can detect subtle asymmetries that may not be apparent clinically. This modality proves particularly valuable when assessing muscle indentations in the context of suspected malignancy or when detailed anatomical localisation is required for surgical planning. The radiation exposure associated with CT scanning necessitates careful consideration of the risk-benefit ratio, particularly in younger patients.
Electromyography and nerve conduction studies provide essential information about the functional integrity of the neuromuscular system when neurological causes are suspected. These studies can differentiate between primary muscle diseases and neurogenic causes of muscle atrophy, whilst also providing prognostic information about the potential for recovery.
The combination of clinical assessment, imaging studies, and electrophysiological testing provides the most comprehensive evaluation of thigh muscle indentations and their
underlying cause remains incomplete without comprehensive treatment planning that addresses both the immediate symptoms and the root pathological process.
Laboratory investigations play a complementary role in the diagnostic workup, particularly when inflammatory or metabolic causes are suspected. Creatine kinase levels can indicate muscle damage, whilst inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein may suggest underlying inflammatory conditions. Specific autoantibody panels become essential when autoimmune myopathies are under consideration, as these can guide targeted therapy and prognosis.
Advanced imaging techniques, including magnetic resonance spectroscopy and diffusion tensor imaging, are emerging as valuable tools for assessing muscle metabolism and microstructural changes. These modalities can detect early pathological changes before visible muscle indentations develop, potentially enabling earlier intervention and improved outcomes. However, their availability remains limited to specialised centres, and their role in routine clinical practice continues to evolve.
The temporal relationship between symptom onset and imaging findings provides crucial diagnostic information. Acute changes typically demonstrate high signal intensity on T2-weighted images, indicating inflammation or oedema, whilst chronic indentations show fatty infiltration and reduced muscle bulk on T1-weighted sequences. This distinction proves essential for determining treatment strategies and predicting potential for recovery.
Functional imaging assessment through dynamic studies can reveal compensatory movement patterns and altered muscle recruitment that may not be apparent during static examination. These findings often correlate with patient-reported functional limitations and can guide targeted rehabilitation interventions designed to restore optimal movement patterns and prevent secondary complications.
The integration of multiple diagnostic modalities creates a comprehensive picture of the underlying pathology responsible for thigh muscle indentations. This multifaceted approach enables clinicians to develop targeted treatment plans that address the specific mechanisms involved, whether they involve neurological dysfunction, inflammatory processes, vascular compromise, or mechanical factors. Early accurate diagnosis remains the cornerstone of successful management, potentially preventing progression of muscle indentations and preserving functional capacity.
Regular monitoring through follow-up imaging studies allows clinicians to assess treatment response and modify therapeutic approaches as needed, ensuring optimal outcomes for patients experiencing thigh muscle indentations.
Understanding the diverse causes of thigh muscle indentations empowers both healthcare professionals and patients to recognise when these changes warrant immediate medical attention versus when they represent benign adaptations to environmental factors. The complexity of potential underlying mechanisms emphasises the importance of thorough evaluation and individualised treatment approaches tailored to each patient’s specific circumstances and functional goals.