Distinguishing between razor burn and herpes simplex virus infection represents one of the most common diagnostic challenges in dermatological practice. Both conditions can manifest as painful, inflamed lesions in intimate areas, creating anxiety and confusion for patients. The ability to accurately differentiate between these conditions is crucial for appropriate treatment and peace of mind. Razor burn, medically termed pseudofolliculitis barbae, affects millions of individuals who engage in regular hair removal, whilst herpes simplex virus infections impact approximately 67% of the global population under 50 years of age. Understanding the distinct characteristics, causes, and progression patterns of each condition empowers you to make informed decisions about seeking medical care and implementing appropriate self-care measures.
Clinical identification of razor burn symptoms and characteristics
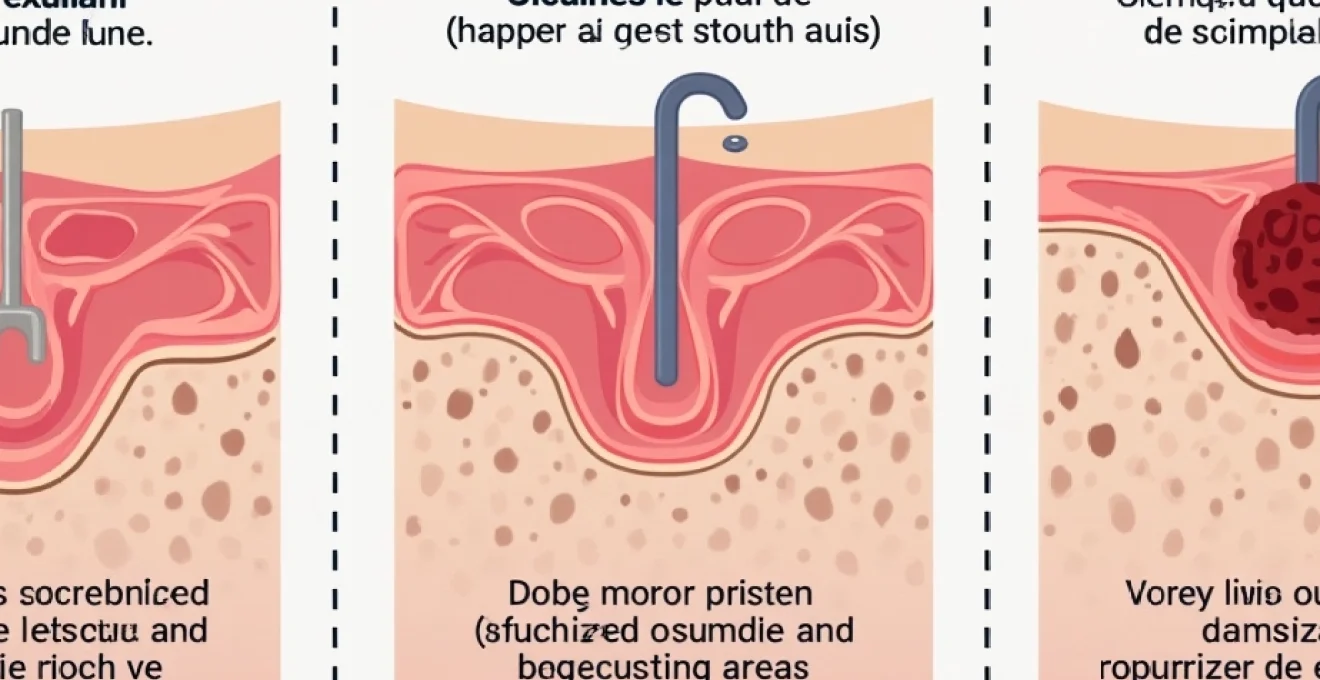
Razor burn manifests as a distinctive inflammatory response following hair removal procedures, characterised by specific morphological features that distinguish it from viral infections. The condition typically presents within hours of shaving, creating a predictable temporal relationship between the grooming activity and symptom onset. Understanding these clinical presentations enables accurate identification and appropriate management strategies for affected individuals.
Follicular inflammation patterns in Post-Shaving dermatitis
The inflammatory response in razor burn centres around individual hair follicles, creating a characteristic pattern of perifollicular erythema and oedema. Each affected follicle becomes surrounded by a zone of redness and swelling, often accompanied by the presence of trapped hair shafts beneath the skin surface. This follicle-centric inflammation distinguishes razor burn from other dermatological conditions, as the inflammatory response directly correlates with hair follicle distribution and density. The severity of inflammation varies based on individual skin sensitivity, hair texture, and shaving technique employed.
Erythematous papule distribution along hair growth lines
Razor burn lesions follow predictable anatomical patterns that correspond to natural hair growth directions and shaving trajectories. The papules and inflamed areas typically align along the paths where razors have been drawn across the skin, creating linear or curved distributions rather than random clustering. This patterned distribution becomes particularly evident in areas where hair growth direction changes, such as the jawline in men or the bikini area in women. The geometric arrangement of lesions provides valuable diagnostic information, as viral infections rarely follow such organised patterns.
Pseudofolliculitis barbae manifestation in sensitive areas
Pseudofolliculitis barbae represents the most severe form of razor burn, particularly affecting individuals with coarse, curly hair who shave frequently. In sensitive areas such as the neck, groin, and axillae, this condition manifests as firm, tender papules that may progress to pustular lesions. The curved nature of certain hair types predisposes these follicles to becoming ingrown, creating a cycle of inflammation and mechanical irritation. Chronic pseudofolliculitis can lead to permanent scarring and hyperpigmentation , making early recognition and appropriate management essential for optimal outcomes.
Temporal onset correlation with shaving frequency and technique
The timing of razor burn symptoms demonstrates a direct correlation with shaving activities, typically manifesting within 2-24 hours post-hair removal. Individuals who shave daily often experience cumulative irritation, whilst those who shave infrequently may notice more pronounced symptoms due to increased hair length and resistance during cutting. Poor shaving technique, including dry shaving, using dull blades, or applying excessive pressure, significantly increases the likelihood and severity of razor burn development. The predictable relationship between grooming activities and symptom onset provides crucial diagnostic information that distinguishes mechanical irritation from infectious processes.
Herpes simplex virus lesion morphology and pathognomonic signs
Herpes simplex virus infections produce characteristic lesions with distinct morphological features that evolve through predictable stages. These viral eruptions demonstrate specific patterns of development, distribution, and associated symptoms that differ markedly from mechanical skin irritation. Recognition of these pathognomonic signs enables accurate diagnosis and appropriate therapeutic intervention during the critical early stages of infection.
HSV-1 and HSV-2 vesicular eruption characteristics
Herpes simplex virus lesions begin as small, clear vesicles filled with viral particles and inflammatory fluid, typically measuring 1-3 millimetres in diameter. These vesicles often appear in characteristic clusters or groups, creating a dewdrop on a rose petal appearance on an erythematous base. HSV-1 infections predominantly affect the orolabial region but can occur genitally through oral-genital contact, whilst HSV-2 primarily manifests in genital and perianal areas. The vesicular stage represents the period of highest viral shedding and transmission risk, making recognition crucial for preventing spread to partners or other body sites.
Prodromal symptoms preceding herpetic outbreak
Many individuals experience characteristic prodromal symptoms 12-48 hours before visible lesions appear, including tingling, burning, or itching sensations at the future eruption site. These neurological symptoms result from viral replication within sensory nerve endings and represent an important diagnostic clue. Systemic prodromal symptoms may include fever, malaise, headache, and regional lymphadenopathy , particularly during initial infections. Recognition of these warning signs enables early antiviral intervention, which can significantly reduce outbreak severity and duration.
Ulcerative lesion progression and crusting phases
Following the vesicular stage, herpes lesions progress through predictable phases of ulceration and crusting over 7-14 days. The vesicles rupture spontaneously or through minor trauma, leaving shallow, painful ulcers with raised, erythematous borders. These ulcerative lesions gradually develop adherent crusts as healing progresses, eventually resolving without scarring in most cases. The ulcerative phase often represents the most painful period of the outbreak, significantly impacting quality of life and daily activities. Unlike razor burn, which typically improves within days, herpetic lesions follow this characteristic progression regardless of external interventions.
Anatomical distribution patterns in primary vs recurrent episodes
Primary herpes infections tend to present with more extensive lesion distribution and severe systemic symptoms compared to recurrent episodes. Initial outbreaks may involve large areas of the genital region, including the external genitalia, perineum, and adjacent skin surfaces. Recurrent episodes typically manifest in more localised patterns, often recurring at the same anatomical sites due to viral dormancy in specific sensory ganglia. The distribution of lesions provides valuable information about the likely transmission route and infection chronicity , helping healthcare providers develop appropriate counselling and treatment strategies.
Viral shedding periods and infectious transmission windows
Herpes simplex virus transmission occurs primarily during active lesion periods, but asymptomatic shedding represents a significant source of infection spread. Viral DNA can be detected in genital secretions for several days before and after visible lesions appear, extending the infectious period beyond clinically apparent symptoms. Peak viral shedding occurs during the vesicular stage, when lesion fluid contains the highest concentration of infectious particles. Understanding these transmission dynamics is crucial for patient education and partner protection strategies, as many transmissions occur during asymptomatic periods when individuals are unaware of their infectious status.
Differential diagnostic criteria between mechanical and viral aetiology
Accurate differentiation between razor burn and herpes requires systematic evaluation of multiple clinical parameters, including lesion morphology, distribution patterns, temporal relationships, and associated symptoms. This diagnostic process involves both clinical observation and laboratory confirmation when uncertainty exists. Understanding the fundamental differences between mechanical irritation and viral infection enables appropriate treatment decisions and prevents unnecessary anxiety or delayed care.
Histopathological examination of affected epithelial tissue
Microscopic examination of affected tissue reveals distinct histological patterns that differentiate mechanical irritation from viral infection. Razor burn demonstrates perifollicular inflammation with neutrophil infiltration, follicular plugging, and reactive epithelial changes without viral cytopathic effects. In contrast, herpes infections show characteristic viral inclusions, multinucleated giant cells, and specific patterns of epithelial necrosis. Biopsy specimens from herpetic lesions reveal ballooning degeneration of keratinocytes and eosinophilic intranuclear inclusions that are pathognomonic for herpes simplex virus infection. Histopathological examination provides definitive diagnostic information when clinical features overlap between conditions.
Tzanck smear cytological analysis for multinucleated giant cells
The Tzanck smear represents a rapid, office-based diagnostic tool for identifying viral cytopathic effects characteristic of herpes infections. This technique involves scraping the base of a fresh vesicle or ulcer and examining the cellular material under microscopic magnification.
Positive Tzanck smears demonstrate multinucleated giant cells with marginated chromatin and ground-glass nuclear appearance, indicating active viral replication within infected keratinocytes.
Whilst this test cannot distinguish between HSV-1 and HSV-2, it provides valuable confirmation of herpetic infection when positive. However, false-negative results occur in up to 30% of cases, particularly in crusted or healing lesions.
PCR testing protocols for HSV DNA detection
Polymerase chain reaction testing represents the gold standard for herpes simplex virus diagnosis, offering superior sensitivity and specificity compared to traditional culture methods. Real-time PCR assays can detect viral DNA even in healing lesions or during periods of low-level viral shedding, providing diagnostic accuracy exceeding 95%. These molecular techniques also enable precise typing of HSV-1 versus HSV-2, which has important implications for prognosis and transmission counselling. PCR testing requires proper specimen collection from vesicular fluid or ulcer base material, with results typically available within 24-48 hours in most clinical settings.
Igg and IgM serological markers in acute vs chronic presentations
Serological testing provides valuable information about infection chronicity and immune status, particularly when lesions are absent or atypical. HSV-specific IgM antibodies indicate recent infection but may persist for several months, limiting their utility for distinguishing acute from recurrent episodes. Type-specific IgG antibodies develop 12-16 weeks after initial infection and persist lifelong , providing information about previous exposure and immune status. Serological testing proves most valuable for asymptomatic individuals seeking to know their HSV status or for confirming chronic infection in patients with atypical presentations.
Professional medical assessment and laboratory confirmation methods
Professional medical evaluation becomes essential when clinical features overlap between razor burn and herpes, particularly in sexually active individuals or those with atypical presentations. Healthcare providers employ systematic assessment protocols that combine clinical examination, patient history, and laboratory testing to establish accurate diagnoses. This comprehensive approach ensures appropriate treatment selection and reduces the risk of misdiagnosis, which can have significant psychological and health implications for affected individuals. Modern diagnostic capabilities enable rapid, accurate identification of viral infections whilst ruling out other potential causes of genital lesions.
Initial medical assessment focuses on detailed history-taking to establish temporal relationships between symptoms and potential triggering factors. Clinicians investigate shaving patterns, sexual activity, previous similar episodes, and associated symptoms to build a comprehensive clinical picture. Physical examination involves careful inspection of lesion morphology, distribution patterns, and surrounding tissue characteristics under adequate lighting conditions. Healthcare providers may utilise dermoscopic examination to identify subtle features such as trapped hairs in follicular lesions or the characteristic appearance of viral vesicles.
Laboratory confirmation methods have evolved significantly with advances in molecular diagnostics, providing rapid and accurate results that guide therapeutic decisions. Many healthcare facilities now offer point-of-care testing that can provide preliminary results within hours of specimen collection.
Modern laboratory protocols include viral culture, molecular amplification techniques, and serological testing, each offering specific advantages depending on the clinical scenario and timing of presentation.
Healthcare providers select appropriate testing modalities based on lesion characteristics, symptom duration, and individual patient factors to maximise diagnostic accuracy.
Documentation of findings and test results creates an important medical record that facilitates future care and monitoring. Accurate diagnosis enables appropriate patient education about condition management, transmission prevention, and long-term prognosis . Healthcare providers also address psychological aspects of diagnosis, particularly when sexually transmitted infections are confirmed, ensuring patients receive comprehensive support and counselling services.
Evidence-based treatment protocols for each condition
Treatment approaches for razor burn and herpes differ fundamentally due to their distinct aetiological mechanisms, requiring targeted therapeutic strategies for optimal outcomes. Razor burn management focuses on reducing inflammation, preventing secondary infection, and promoting healing through supportive care measures. Herpes treatment involves antiviral therapy to suppress viral replication, symptom management, and strategies to prevent transmission and recurrent episodes. Understanding evidence-based protocols for each condition ensures appropriate therapeutic selection and maximises treatment effectiveness.
Razor burn treatment typically begins with immediate cessation of hair removal activities in affected areas to allow tissue recovery and inflammation resolution. Topical interventions include cool compresses to reduce erythema and oedema, followed by application of fragrance-free moisturisers or barrier creams to protect healing tissue. Anti-inflammatory agents such as topical corticosteroids may provide symptom relief but should be used judiciously to avoid skin thinning or delayed healing . Severe cases with secondary bacterial infection may require topical or systemic antibiotic therapy to prevent progression to cellulitis or abscess formation.
Herpes simplex virus treatment protocols emphasise early antiviral intervention to reduce outbreak severity and duration whilst preventing complications. First-line antiviral agents include aciclovir, valaciclovir, and famciclovir, with dosing regimens adjusted based on infection chronicity and patient immune status. Episodic therapy involves treating individual outbreaks with short courses of antiviral medication, whilst suppressive therapy provides continuous medication for individuals with frequent recurrences. Pain management may require topical anaesthetics or systemic analgesics, particularly during the acute ulcerative phase.
Long-term management strategies differ significantly between conditions, with razor burn focusing on prevention through improved shaving techniques and herpes requiring ongoing monitoring and transmission counselling. Patients with recurrent razor burn benefit from alternative hair removal methods such as laser therapy or chemical depilatories that reduce mechanical trauma.
Herpes management involves comprehensive patient education about transmission risks, outbreak recognition, and partner notification protocols to prevent disease spread.
Regular follow-up care enables monitoring for treatment effectiveness and adjustment of therapeutic regimens based on individual response patterns.
Prevention strategies and risk mitigation techniques
Effective prevention strategies for razor burn and herpes focus on addressing the underlying risk factors and transmission mechanisms specific to each condition. Razor burn prevention emphasises proper shaving technique, skin preparation, and equipment maintenance to minimise mechanical trauma and inflammatory responses. Herpes prevention involves reducing transmission risks through barrier protection methods, partner screening, and behavioural modifications during infectious periods. Implementing comprehensive prevention strategies significantly reduces the likelihood of developing either condition and improves overall skin health outcomes.
Optimal shaving technique forms the cornerstone of razor burn prevention, beginning with proper skin preparation through warm water exposure and application of appropriate lubricating products. Pre-shave oils help soften hair shafts and create a protective barrier between the razor and skin surface , reducing friction and irritation during hair removal. Sharp, clean razor blades should be used with gentle pressure, following natural hair growth direction rather than shaving against the grain. Post-shave care involves immediate application of alcohol-free aftershave products or moisturisers to soothe irritated tissue and maintain skin barrier function.
Alternative hair removal methods offer effective solutions for individuals prone to recurrent razor burn, including electric clippers that trim hair without close contact with skin, chemical depilatories that dissolve hair proteins, or laser hair removal for permanent hair reduction. IPL (Intense Pulsed Light) therapy provides long-lasting hair reduction with minimal skin irritation for suitable candidates. Regular exfoliation using gentle mechanical or chemical methods helps prevent ingrown hairs by removing dead skin cells that can trap emerging hair shafts.
Herpes prevention strategies focus on reducing transmission risks through consistent barrier protection during sexual activity and avoiding contact during symptomatic periods. Latex or polyurethane condoms provide significant protection against HSV transmission, though they do not eliminate risk entirely due to potential viral shedding from uncovered areas. Regular STI screening for sexually active individuals enables early detection and treatment of infections before symptom development. Partner notification and testing protocols help identify asymptomatic carriers and implement appropriate prevention measures within relationships.
Stress management and immune system support play important roles in preventing herpes recurrences, as psychological stress and immunosuppression can trigger viral reactivation. Adequate sleep, regular exercise, and stress reduction techniques help maintain immune system function and reduce outbreak frequency
in chronic herpes patients. Nutritional support through adequate vitamin intake, particularly vitamins C, E, and zinc, contributes to optimal immune function and tissue healing capacity. Avoiding known triggers such as excessive UV exposure, hormonal fluctuations, or specific foods helps prevent viral reactivation in susceptible individuals.
Educational initiatives focusing on accurate information about transmission risks, symptom recognition, and prevention strategies help reduce stigma and promote responsible sexual health behaviours. Community health programs that provide accessible testing and counselling services play crucial roles in controlling herpes transmission rates. Regular healthcare provider consultations enable monitoring of prevention strategy effectiveness and adjustment of recommendations based on individual risk factors and lifestyle changes. Healthcare providers should emphasise that both conditions are manageable with appropriate care and that seeking professional guidance early in the course of symptoms leads to optimal outcomes.
Technology-assisted prevention tools, including smartphone applications for tracking symptoms or outbreak patterns, provide valuable data for managing recurrent conditions. Telemedicine consultations offer discreet access to healthcare services for individuals concerned about privacy or accessibility issues. Digital health platforms increasingly provide educational resources, symptom trackers, and direct communication channels with healthcare providers, enhancing overall disease management and prevention efforts. These modern approaches complement traditional prevention strategies and improve patient engagement in their ongoing healthcare management.