Discovering a small white bump in your throat can be an unsettling experience that prompts immediate concern about your health. These mysterious lesions, ranging from barely visible spots to more prominent raised areas, affect millions of people worldwide and can arise from various underlying conditions. While the appearance of white throat bumps often triggers anxiety about serious medical conditions, the vast majority of these lesions are benign and treatable with appropriate medical intervention.
The throat’s complex anatomical structure, comprising the pharynx, tonsils, and surrounding lymphatic tissue, creates numerous opportunities for different types of lesions to develop. Understanding the diverse aetiologies behind these white formations enables both patients and healthcare professionals to approach diagnosis and treatment more effectively. From simple inflammatory responses to complex infectious processes, the causes of throat bumps span a broad spectrum of medical conditions that require careful evaluation and targeted therapeutic approaches.
Infectious aetiologies behind palatine and pharyngeal white lesions
Infectious agents represent the most common underlying cause of white bumps appearing in the throat region. These pathogens, including bacteria, viruses, and fungi, create inflammatory responses that manifest as visible lesions on the throat’s mucosal surfaces. The body’s immune response to these infectious agents often results in the characteristic white or yellowish appearance that patients observe when examining their throats.
Streptococcal pharyngitis and tonsillar exudate formation
Streptococcal pharyngitis, commonly known as strep throat, frequently presents with distinctive white patches or bumps on the tonsils and posterior pharynx. Group A Streptococcus bacteria colonise the throat tissues, triggering an intense inflammatory response that produces purulent exudate. This bacterial infection affects approximately 15-30% of childhood pharyngitis cases and 5-15% of adult cases, making it a significant contributor to white throat lesions.
The characteristic appearance of streptococcal throat lesions includes white or greyish patches that may appear raised above the surrounding tissue surface. These formations typically accompany severe throat pain, difficulty swallowing, and systemic symptoms such as fever and malaise. The exudate formation results from neutrophil infiltration and bacterial toxin production, creating the distinctive white appearance that helps distinguish bacterial from viral pharyngitis.
Epstein-barr virus mononucleosis and palatal petechiae
Infectious mononucleosis, primarily caused by the Epstein-Barr virus, produces characteristic white lesions throughout the oropharynx. This viral infection commonly affects adolescents and young adults, creating a constellation of symptoms that includes throat pain, lymphadenopathy, and distinctive oral manifestations. The virus’s tropism for lymphatic tissue results in significant tonsillar enlargement and exudate formation that can appear as white bumps or patches.
Palatal petechiae, small red or white spots on the soft palate, represent another hallmark of mononucleosis that patients may interpret as throat bumps. These lesions develop due to capillary fragility and platelet dysfunction associated with the viral infection. The combination of tonsillar exudate and palatal lesions creates a characteristic appearance that experienced clinicians readily recognise as indicative of mononucleosis.
Candida albicans oropharyngeal thrush manifestations
Oropharyngeal candidiasis, or thrush, manifests as white plaques that can appear as raised bumps throughout the mouth and throat. This fungal infection predominantly affects immunocompromised patients, infants, elderly individuals, and those receiving antibiotic therapy. Candida albicans organisms adhere to mucosal surfaces, forming biofilms that appear as characteristic white, cottage cheese-like lesions.
The fungal plaques associated with thrush typically wipe away when scraped, revealing an erythematous base underneath. This distinguishing feature helps differentiate candidal lesions from other causes of white throat bumps. Patients with diabetes mellitus, HIV infection, or those using inhaled corticosteroids demonstrate increased susceptibility to developing these distinctive white fungal formations in their throats.
Herpetic stomatitis and vesicular throat eruptions
Herpes simplex virus infections can produce vesicular lesions in the throat that initially appear as small, fluid-filled bumps before rupturing and developing white or greyish centres. Primary herpetic gingivostomatitis particularly affects children and young adults, creating painful vesicles throughout the oral cavity and throat. These lesions typically begin as small, clear vesicles that rapidly progress to ulcerative lesions with white fibrinous bases.
The vesicular nature of herpetic lesions distinguishes them from bacterial exudates, as they represent focal areas of epithelial necrosis rather than inflammatory exudate accumulation. Patients often describe intense pain associated with these lesions, and the characteristic clustering pattern helps clinicians recognise viral aetiology. Recurrent herpes simplex infections may produce similar but typically less extensive lesions in previously affected individuals.
Benign neoplastic and cystic throat formations
Non-infectious causes of white throat bumps encompass a diverse range of benign growths and cystic formations. These lesions develop through various mechanisms, including ductal obstruction, reactive hyperplasia, and benign neoplastic processes. Understanding these conditions helps distinguish them from infectious causes and guides appropriate treatment decisions.
Retention cysts of minor salivary glands
Mucous retention cysts frequently develop when minor salivary gland ducts become obstructed, resulting in fluid accumulation and cyst formation. These benign lesions appear as smooth, dome-shaped bumps with a characteristic bluish-white or translucent appearance. The cysts commonly occur on the soft palate, buccal mucosa, and posterior pharynx, where numerous minor salivary glands are distributed.
The pathogenesis involves mechanical obstruction of salivary ducts due to trauma, inflammation, or debris accumulation. As secretions continue to be produced but cannot drain normally, pressure builds within the duct system, eventually leading to cyst formation. These lesions typically remain asymptomatic unless they reach significant size or become secondarily infected. Surgical excision provides definitive treatment, though small cysts may resolve spontaneously if the obstruction clears.
Squamous papilloma and HPV-Associated growths
Human papillomavirus (HPV) infection can produce benign squamous papillomas that appear as white, warty growths in the throat. These lesions most commonly result from HPV types 6 and 11, which demonstrate low oncogenic potential but can cause significant local symptoms. The papillomas typically exhibit a characteristic “mulberry” or “cauliflower” appearance with a white or pink coloration.
Papillomas may occur as solitary lesions or present as multiple growths throughout the upper aerodigestive tract. While generally benign, these lesions can cause voice changes, throat discomfort, and difficulty swallowing when located in critical anatomical areas. The potential for malignant transformation, though rare, necessitates complete excision and histopathological examination of all suspected papillomatous lesions.
Fibroma and reactive hyperplastic tissue
Reactive fibrous hyperplasia represents a common response to chronic irritation or trauma in the throat region. These lesions appear as firm, smooth bumps with a white or pink surface, typically measuring several millimetres in diameter. Unlike true neoplasms, fibromas represent reactive tissue proliferation in response to persistent mechanical irritation.
Common causes of reactive fibrous hyperplasia include chronic coughing, throat clearing, gastroesophageal reflux, and mechanical trauma from foreign objects or medical procedures. The lesions consist primarily of mature fibrous connective tissue covered by normal or slightly thickened epithelium.
While fibromas are entirely benign, their presence often indicates an underlying source of chronic irritation that should be identified and addressed to prevent recurrence.
Lymphoepithelial cysts in palatine tonsils
Lymphoepithelial cysts occasionally develop within the palatine tonsils, appearing as small, white or yellow bumps on the tonsillar surface. These cysts form when epithelial remnants become trapped within lymphoid tissue during normal tonsillar development. The cysts contain keratin debris and cellular material, giving them a characteristic white or yellowish appearance.
These benign formations typically remain small and asymptomatic, though larger cysts may cause a sensation of fullness or foreign body sensation in the throat. The cysts can be distinguished from infectious processes by their persistent appearance and lack of associated inflammatory symptoms. Most lymphoepithelial cysts require no treatment unless they cause significant symptoms or cosmetic concerns.
Inflammatory and autoimmune oral pathology
Inflammatory and autoimmune conditions can produce white lesions in the throat that may appear as raised bumps or patches. These conditions often involve complex immunological processes that result in chronic inflammation and tissue damage. Lichen planus represents one of the most common autoimmune conditions affecting the oral cavity, manifesting as white, lacy lesions or erosive areas throughout the mouth and throat. The condition results from T-cell mediated destruction of basal epithelial cells, creating characteristic histopathological findings and clinical presentations.
Pemphigus vulgaris and bullous pemphigoid, though rare, can produce vesicular lesions in the throat that subsequently develop white fibrinous bases after rupture. These autoimmune blistering diseases require prompt recognition and treatment to prevent serious complications. The lesions typically demonstrate positive Nikolsky sign and require immunofluorescence studies for definitive diagnosis. Systemic immunosuppressive therapy forms the cornerstone of treatment for these potentially life-threatening conditions.
Chronic granulomatous inflammation, such as that seen in Crohn’s disease or sarcoidosis, can occasionally produce white nodular lesions in the throat. These conditions represent systemic diseases with oral manifestations that may precede other systemic symptoms. The granulomatous inflammation creates characteristic histopathological patterns that help distinguish these conditions from infectious or neoplastic processes. Recognition of oral manifestations of systemic inflammatory diseases enables earlier diagnosis and treatment of the underlying condition.
Traumatic and mechanical throat lesion development
Mechanical trauma and chronic irritation frequently contribute to the development of white lesions in the throat region. These traumatic injuries can result from acute incidents or chronic repetitive irritation that leads to tissue damage and subsequent healing responses. Understanding the relationship between trauma and lesion development helps clinicians identify preventable causes and implement appropriate treatment strategies.
Thermal burns from hot foods or beverages can create white, sloughing lesions in the throat that may persist for several days to weeks. The initial thermal injury damages the epithelial layer, leading to coagulation necrosis and the formation of white eschar tissue. As healing progresses, the white necrotic tissue gradually separates, revealing healthy underlying epithelium. Severe thermal injuries may require medical intervention to prevent secondary infection and promote proper healing.
Chemical burns from household cleaners, medications, or caustic substances can produce more severe white lesions with deeper tissue penetration. These injuries often require immediate medical attention to assess the extent of damage and prevent complications such as stricture formation or secondary infection. The severity of chemical burns depends on the specific agent involved, concentration, and duration of exposure.
Prompt irrigation and neutralisation of chemical agents can significantly reduce the extent of tissue damage and improve healing outcomes.
Chronic mechanical irritation from ill-fitting dental appliances, sharp tooth edges, or repetitive behaviours such as cheek biting can lead to the development of white, thickened areas known as hyperkeratosis. These lesions represent the tissue’s attempt to protect itself from ongoing trauma through increased keratin production. While generally benign, chronic hyperkeratotic lesions require elimination of the irritating factor to prevent progression and potential malignant transformation in rare cases.
Differential diagnosis through clinical examination techniques
Accurate diagnosis of white throat bumps requires systematic clinical evaluation combining visual examination, palpation, and appropriate diagnostic testing. The clinical assessment begins with a comprehensive history focusing on symptom onset, duration, associated symptoms, and relevant medical history. Understanding the patient’s immunological status, medication usage, and environmental exposures provides crucial context for interpreting physical findings.
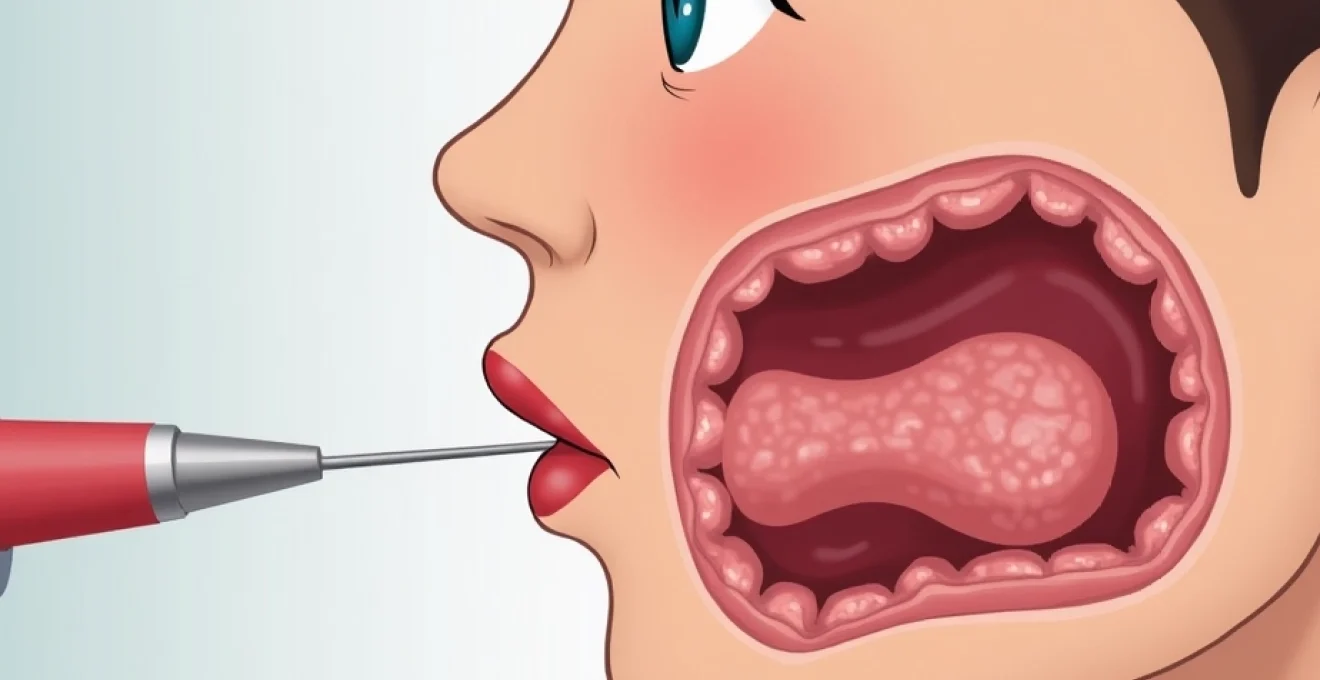
Visual inspection represents the cornerstone of throat lesion evaluation, requiring adequate lighting and appropriate positioning to visualise all anatomical structures. Clinicians should systematically examine the lips, buccal mucosa, tongue, floor of mouth, hard and soft palates, tonsillar pillars, posterior pharynx, and visible laryngeal structures. The use of indirect laryngoscopy or flexible fibreoptic endoscopy may be necessary to fully evaluate lesions in posterior locations or when patient cooperation limits visual access.
Palpation techniques provide valuable information about lesion consistency, mobility, and relationship to underlying structures. Soft, fluctuant lesions typically suggest cystic formations or abscesses, while firm, fixed lesions may indicate fibrous tissue or more concerning pathology. The presence or absence of regional lymphadenopathy provides additional diagnostic information and may influence treatment decisions. Bilateral palpation of cervical lymph node chains should be performed systematically to detect subtle asymmetries or enlargement.
Laboratory investigations may be warranted based on clinical suspicions raised during the physical examination. Throat cultures or rapid antigen detection tests help identify bacterial pathogens in cases suggesting infectious aetiology. Complete blood count with differential can reveal evidence of viral infections such as mononucleosis through the presence of atypical lymphocytes. Fungal cultures or potassium hydroxide preparations assist in diagnosing candidal infections, particularly in immunocompromised patients or those with predisposing factors.
Biopsy considerations become important when lesions persist despite appropriate treatment, demonstrate concerning features, or present in high-risk patients. The decision to pursue tissue sampling should balance the potential diagnostic yield against procedural risks and patient factors. Incisional biopsy typically suffices for larger lesions, while small lesions may undergo excisional biopsy for complete removal and diagnosis. Proper handling of tissue specimens, including appropriate fixation and communication with pathologists, ensures optimal diagnostic accuracy.
Treatment protocols and management strategies for benign throat lesions
Treatment approaches for white throat bumps must be tailored to the specific underlying aetiology identified through clinical evaluation and diagnostic testing. Conservative management often suffices for benign lesions, while infectious causes may require targeted antimicrobial therapy. The selection of appropriate treatment modalities depends on lesion characteristics, patient symptoms, and individual risk factors that may influence treatment outcomes.
Conservative management strategies form the foundation of treatment for many benign throat lesions. These approaches include avoiding mechanical irritants, maintaining good oral hygiene, and using topical anaesthetics for symptomatic relief. Warm salt water gargles provide gentle cleansing action and may help reduce inflammation in some cases. Patients should be advised to avoid spicy foods, alcohol, and tobacco products that may exacerbate throat irritation and delay healing processes.
Antimicrobial therapy becomes necessary when infectious aetiologies are confirmed or strongly suspected based on clinical presentation. Bacterial infections such as streptococcal pharyngitis require appropriate antibiotic treatment, with penicillin remaining the first-line choice for Group A Streptococcus infections. Alternative antibiotics such as azithromycin or cephalexin may be used in penicillin-allergic patients, though resistance patterns should be considered when selecting alternative agents.
Antifungal medications are indicated for confirmed candidal infections, with topical agents such as nystatin or clotrimazole often providing effective treatment for localised infections. Systemic antifungal therapy may be necessary for immunocompromised patients or those with extensive disease. The duration of antifungal treatment typically ranges from 7-14 days, though longer courses may be required in certain clinical situations.
Surgical intervention becomes necessary for lesions that fail to respond to conservative management, cause significant symptoms, or demonstrate concerning features requiring tissue diagnosis.
Minor surgical procedures such as excision or laser ablation can be performed in office settings for most benign lesions, providing both therapeutic benefit and definitive histopathological diagnosis.
Post-operative care instructions should emphasise wound care, activity restrictions, and signs requiring immediate medical attention.
Follow-up protocols ensure proper healing and detect any concerning changes in lesion appearance or patient symptoms. Patients should be instructed to return for re-evaluation if symptoms worsen, new lesions develop, or healing does not progress as expected. Long-term monitoring may be appropriate for patients with recurrent lesions or underlying conditions predisposing to throat pathology. The development of standardised follow-up
protocols enables healthcare providers to track treatment effectiveness and identify patterns that may influence future management decisions.
Patient education plays a crucial role in successful treatment outcomes, as understanding the nature of throat lesions helps reduce anxiety and improve compliance with treatment recommendations. Patients should receive clear explanations about their diagnosis, expected treatment duration, and potential complications that may require immediate medical attention. Written instructions regarding medication usage, activity restrictions, and follow-up care provide valuable reference materials that patients can consult at home.
Prevention strategies should be discussed with patients who experience recurrent throat lesions or those with identifiable risk factors. These may include modifications to oral hygiene routines, dietary adjustments, environmental changes, or treatment of underlying medical conditions that predispose to lesion development. The implementation of comprehensive preventive measures often proves more effective than repeated treatment of recurrent lesions.
Multidisciplinary care coordination may be necessary for complex cases involving systemic diseases or patients with multiple comorbidities. Collaboration between primary care providers, otolaryngologists, dermatologists, and other specialists ensures comprehensive evaluation and optimal treatment outcomes. The development of clear communication channels between healthcare team members facilitates efficient care delivery and reduces the risk of treatment delays or conflicts.
Quality assurance measures should be implemented to monitor treatment outcomes and identify opportunities for improvement in clinical care protocols. Regular review of patient outcomes, complication rates, and satisfaction scores provides valuable feedback for refining treatment approaches. The integration of evidence-based practices with clinical experience creates optimal treatment protocols that can be adapted to individual patient needs and institutional capabilities.
Cost-effectiveness considerations become increasingly important in healthcare delivery, requiring careful evaluation of treatment options that balance clinical effectiveness with economic sustainability. Simple conservative measures often provide excellent outcomes at minimal cost, while more expensive interventions should be reserved for cases where simpler approaches prove inadequate. The development of treatment algorithms that prioritise cost-effective interventions while maintaining high-quality care serves both patient and institutional interests.
Documentation requirements must be carefully maintained throughout the treatment process to ensure continuity of care and provide legal protection for healthcare providers. Detailed records should include initial presentation, diagnostic findings, treatment decisions, patient responses, and any complications encountered during the care process. Standardised documentation templates can improve consistency and completeness while reducing the administrative burden on clinical staff.
Research opportunities continue to emerge in the field of oral and throat pathology, offering potential for improved diagnostic techniques and treatment modalities. Participation in clinical research studies may provide patients with access to cutting-edge treatments while contributing to the advancement of medical knowledge. Healthcare providers should stay informed about ongoing research developments and consider referring appropriate patients to research centres when beneficial opportunities arise.
The integration of telemedicine technologies offers new possibilities for follow-up care and patient monitoring, particularly for patients with limited access to specialised healthcare facilities. Remote consultation capabilities allow for visual assessment of healing progress and provide patients with convenient access to expert medical advice. However, the limitations of remote evaluation must be clearly understood, and patients should be educated about circumstances requiring in-person medical evaluation.