The sensation of ear fullness can be frustrating and concerning, particularly when it persists despite the absence of any apparent ear infection or blockage. For many individuals experiencing this discomfort, the root cause may lie not within the ear itself, but in the intricate relationship between the temporomandibular joint and the auditory system. Understanding this connection is crucial for proper diagnosis and effective treatment, as traditional approaches to ear-related symptoms may prove inadequate when the underlying issue stems from TMJ dysfunction.
The temporomandibular joint serves as a complex hinge mechanism that facilitates essential functions such as speaking, chewing, and yawning. When this joint experiences dysfunction, the effects can extend far beyond jaw discomfort, potentially manifesting as a range of auricular symptoms that mimic primary ear disorders. This interconnected relationship between jaw mechanics and auditory perception represents a fascinating example of how anatomical proximity can create unexpected clinical presentations.
Temporomandibular joint anatomy and its proximity to the middle ear
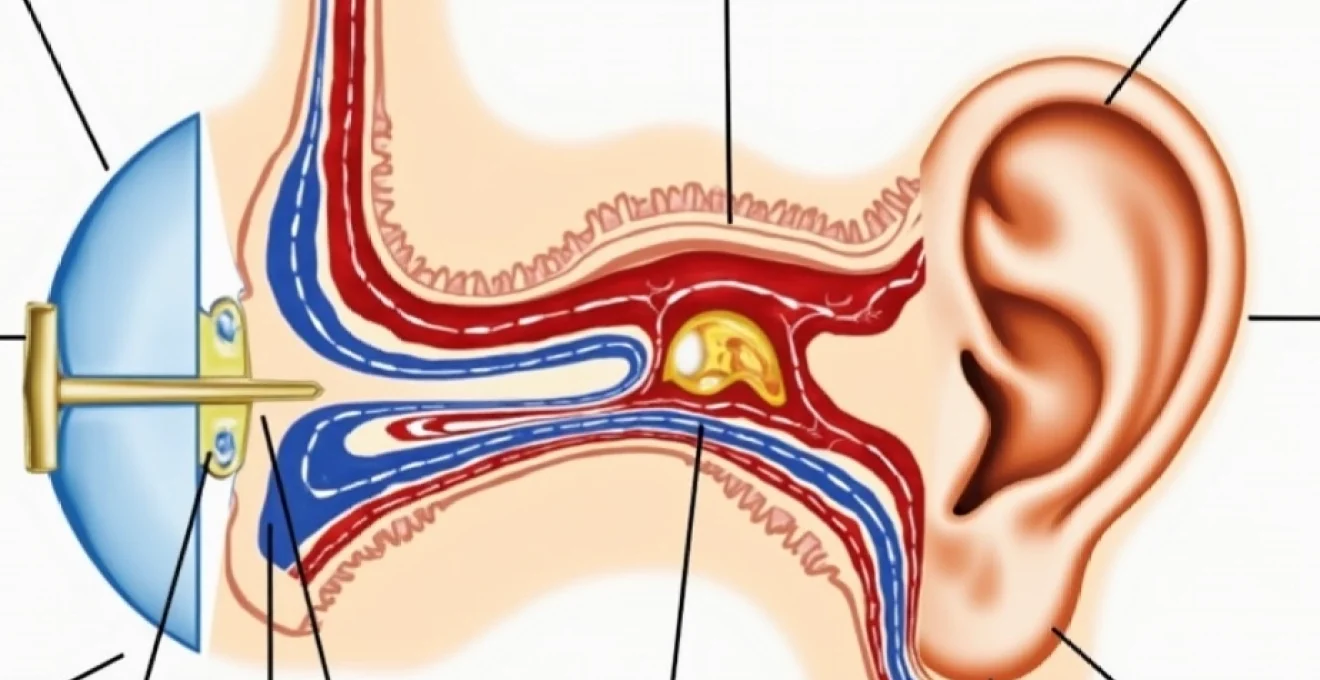
The anatomical relationship between the temporomandibular joint and the ear represents one of the most intricate examples of structural interdependence in the human body. Located just anterior to the external auditory canal, the TMJ shares critical anatomical boundaries with several components of the auditory system. This proximity creates a unique situation where dysfunction in one area can directly influence the function of neighbouring structures, leading to complex symptom patterns that challenge traditional diagnostic approaches.
Mandibular condyle position relative to the auditory canal
The mandibular condyle, which forms the movable portion of the temporomandibular joint, sits in remarkably close proximity to the external auditory canal. When jaw dysfunction occurs, changes in condylar position can create pressure variations that directly impact the ear’s internal environment. This spatial relationship means that even subtle alterations in jaw alignment can produce significant effects on auditory perception and comfort.
During normal jaw function, the condyle moves smoothly within the glenoid fossa, maintaining appropriate spacing from auditory structures. However, when TMJ dysfunction develops, this delicate balance becomes disrupted. Condylar displacement can create mechanical pressure that interferes with normal ear function, potentially leading to sensations of fullness, pressure, or even pain within the auditory canal.
Trigeminal nerve branch interconnections with auricular structures
The trigeminal nerve system provides a crucial neurological bridge between the temporomandibular joint and the auditory system. Branch connections from this extensive nerve network create pathways through which TMJ dysfunction can manifest as ear-related symptoms. The auriculotemporal nerve, a branch of the mandibular division of the trigeminal nerve, innervates both TMJ structures and portions of the external ear, creating direct neurological connections between these anatomically distinct regions.
When TMJ inflammation or dysfunction occurs, neural pathway sensitisation can lead to referred pain patterns that manifest as ear discomfort. This neurological crosstalk explains why individuals with TMJ disorders often experience ear pain without any underlying ear pathology. Understanding these nerve interconnections is essential for clinicians attempting to differentiate between primary ear disorders and TMJ-related auricular symptoms.
Eustachian tube function and TMJ muscular influence
The Eustachian tube plays a vital role in maintaining proper middle ear pressure and drainage. Muscles involved in TMJ function, particularly the tensor veli palatini, also influence Eustachian tube opening and closing mechanisms. When jaw muscles become tense or dysfunctional due to TMJ disorders, their altered function can directly impact Eustachian tube performance, leading to pressure imbalances and the characteristic sensation of ear fullness.
Research indicates that muscle tension patterns associated with TMJ dysfunction can prevent proper Eustachian tube opening during swallowing or yawning. This functional impairment creates a cascade of effects, including reduced middle ear ventilation, pressure accumulation, and the development of auricular symptoms that closely mimic primary ear pathology. The relationship between jaw muscle function and Eustachian tube performance represents a critical connection in understanding TMJ-related ear complaints.
Retrodiscal tissue inflammation effects on otic capsule
The retrodiscal tissues of the temporomandibular joint contain numerous blood vessels and nerve endings that can become inflamed during TMJ dysfunction. This inflammation can create pressure effects that extend beyond the joint capsule, potentially impacting nearby auditory structures including the otic capsule. The proximity of these tissues means that inflammatory processes within the TMJ can directly influence the biomechanical environment surrounding the inner ear.
When retrodiscal tissue inflammation occurs, the resulting swelling and pressure changes can affect the delicate balance of forces acting upon the otic capsule. This mechanical disruption may contribute to alterations in inner ear function, potentially explaining why some individuals with TMJ disorders experience not only ear fullness but also balance disturbances and auditory perception changes.
Neurological pathways connecting TMJ dysfunction to auricular symptoms
The neurological connections between the temporomandibular joint and the auditory system represent a complex network of sensory and motor pathways that can transmit dysfunction signals across anatomical boundaries. Understanding these neurological relationships is essential for comprehending how TMJ disorders can manifest as ear-related symptoms, often creating diagnostic challenges for healthcare providers unfamiliar with these interconnections.
Mylohyoid nerve referred pain patterns to tympanic membrane
The mylohyoid nerve, a branch of the inferior alveolar nerve, provides sensory innervation to structures associated with the temporomandibular joint and can create referred pain patterns that affect tympanic membrane sensation. When TMJ dysfunction creates nerve irritation or sensitisation, pain signals can be referred along these neural pathways, creating the perception of ear pain or discomfort even when the tympanic membrane itself remains healthy.
Clinical observations suggest that referred pain mechanisms through the mylohyoid nerve pathway can create surprisingly convincing ear-related symptoms. Patients often describe sensations of ear pain, pressure, or fullness that closely mimic primary ear disorders, making differential diagnosis particularly challenging without careful consideration of TMJ involvement.
Auriculotemporal nerve compression mechanisms
The auriculotemporal nerve travels in close proximity to the temporomandibular joint and can become compressed or irritated when joint dysfunction occurs. This nerve provides sensory innervation to the external ear, temporal region, and portions of the TMJ capsule, creating a direct neurological link between jaw dysfunction and ear symptoms. Compression of this nerve can lead to altered sensation, pain, or numbness affecting both the jaw and ear regions simultaneously.
When TMJ dysfunction creates swelling or structural changes within the joint, the auriculotemporal nerve may become mechanically compressed, leading to neurological dysfunction that manifests as ear-related symptoms. Understanding this compression mechanism is crucial for developing effective treatment strategies that address the root cause of symptoms rather than merely treating the ear-related manifestations.
Sphenomandibular ligament tension impact on tensor tympani muscle
The sphenomandibular ligament provides structural support for the temporomandibular joint and can influence the function of the tensor tympani muscle through shared anatomical connections. When TMJ dysfunction creates abnormal tension within this ligament system, the resulting mechanical changes can affect tensor tympani muscle function, potentially leading to alterations in middle ear mechanics and the development of ear-related symptoms.
Increased tension within the sphenomandibular ligament can create a mechanical coupling effect that influences tensor tympani muscle tone and function. This relationship may explain why some individuals with TMJ disorders experience acoustic sensitivity or altered sound perception, as the tensor tympani muscle plays a crucial role in protecting the inner ear from excessive sound exposure.
Cervical sympathetic chain dysfunction in TMJ-Related otalgia
The cervical sympathetic chain provides autonomic innervation to structures of the head and neck, including components of both the temporomandibular joint and the auditory system. When TMJ dysfunction creates muscle tension or postural changes that affect cervical spine alignment, secondary effects on the sympathetic chain can occur, potentially leading to autonomic dysfunction that manifests as ear-related symptoms.
Sympathetic chain dysfunction can affect vascular tone and glandular function within the ear, potentially contributing to sensations of fullness, pressure, or discomfort. This autonomic component of TMJ-related ear symptoms represents an often-overlooked aspect of the condition that may require specific therapeutic interventions targeting sympathetic nervous system function .
Muscular dysfunctions in TMJ disorders affecting auditory perception
The muscular system surrounding the temporomandibular joint extends far beyond the primary muscles of mastication, encompassing a complex network of interconnected muscle groups that can influence auditory function when dysfunction occurs. These muscular relationships create multiple pathways through which TMJ disorders can impact ear-related symptoms, often producing effects that extend throughout the head and neck region.
The masseter, temporalis, medial pterygoid, and lateral pterygoid muscles work in coordinated fashion during normal jaw function. When TMJ dysfunction develops, these muscles may develop trigger points, spasms, or chronic tension patterns that can affect nearby structures including those involved in hearing and balance. Muscle hypertonicity associated with TMJ disorders can create pressure effects that extend beyond the immediate area of dysfunction, potentially impacting Eustachian tube function and middle ear mechanics.
Secondary muscle groups, including the sternocleidomastoid, scalene, and suboccipital muscles, often develop compensatory tension patterns in response to primary TMJ dysfunction. These secondary effects can create a complex web of muscular imbalances that may contribute to cervical spine dysfunction, altered head posture, and subsequent changes in auditory system function. The interconnected nature of these muscle systems means that effective treatment often requires addressing multiple muscle groups rather than focusing solely on the primary muscles of mastication.
Myofascial trigger points within TMJ-related muscles can create referred pain patterns that extend to the ear region, producing sensations that closely mimic primary ear disorders. These trigger points may develop in response to acute injury, chronic overuse, or sustained muscle tension, and can persist long after the initial cause of dysfunction has resolved. Understanding the myofascial component of TMJ-related ear symptoms is essential for developing comprehensive treatment approaches that address both the muscular and articular aspects of the disorder.
The relationship between jaw muscle dysfunction and ear symptoms represents one of the most underrecognised connections in clinical medicine, often leading to misdiagnosis and inappropriate treatment approaches.
Clinical manifestations of TMJ-Induced ear fullness and pressure
The clinical presentation of TMJ-induced ear symptoms can vary significantly between individuals, often creating diagnostic challenges due to the similarity between these symptoms and those associated with primary ear disorders. Understanding the specific characteristics of TMJ-related ear complaints is essential for accurate diagnosis and appropriate treatment planning. These symptoms often fluctuate in intensity and may correlate with jaw activity, stress levels, or postural changes, providing important diagnostic clues for clinicians familiar with TMJ-ear relationships.
Aural pressure sensation grading using visual analogue scales
Quantifying the severity of ear pressure sensations associated with TMJ dysfunction requires standardised assessment tools that can capture the subjective nature of these symptoms. Visual analogue scales provide a reliable method for documenting symptom intensity and tracking changes over time. Patients typically describe TMJ-related ear pressure as ranging from mild fullness to severe, debilitating pressure that significantly impacts daily activities and quality of life.
The pattern of pressure sensation in TMJ-related ear complaints often differs from that seen in primary ear disorders. TMJ-induced pressure may fluctuate throughout the day, often correlating with jaw activity, stress levels, or specific postures. This variability contrasts with the more consistent pressure patterns typically seen in conditions such as Eustachian tube dysfunction or middle ear pathology, providing important diagnostic information for experienced clinicians.
Tinnitus frequency patterns in temporomandibular dysfunction
Tinnitus associated with TMJ dysfunction often exhibits specific frequency characteristics that can help differentiate it from tinnitus caused by primary auditory system pathology. TMJ-related tinnitus frequently presents as low-frequency sounds, such as rumbling, buzzing, or humming, rather than the high-pitched ringing commonly associated with hearing loss or ototoxic medications. The intensity and character of TMJ-related tinnitus may change with jaw movement, muscle tension, or stress levels.
The temporal pattern of TMJ-related tinnitus also provides diagnostic clues. Many patients report that their tinnitus worsens during periods of increased jaw clenching or grinding, particularly during sleep or times of stress. Some individuals notice that specific jaw movements or positions can temporarily modify or eliminate their tinnitus, suggesting a direct mechanical relationship between jaw function and auditory perception .
Hearing threshold fluctuations during jaw movement testing
Audiometric testing during jaw movement can reveal characteristic patterns of hearing threshold fluctuation in patients with TMJ-related auditory symptoms. These fluctuations typically affect low-frequency hearing more significantly than high-frequency thresholds, reflecting the mechanical nature of the underlying dysfunction. The degree of threshold shift may correlate with the severity of TMJ dysfunction and can provide objective evidence of the relationship between jaw mechanics and auditory function.
Dynamic audiometry, performed while the patient engages in specific jaw movements, can demonstrate real-time changes in hearing sensitivity associated with temporomandibular joint position. These findings can be particularly valuable in cases where standard audiometric testing appears normal, but patients continue to report hearing-related complaints that correlate with their TMJ symptoms.
Vestibular symptoms associated with TMJ disc displacement
Vestibular symptoms, including dizziness, vertigo, and balance disturbances, can occur in association with TMJ disorders, particularly when disc displacement or severe joint dysfunction is present. The proximity of the temporomandibular joint to vestibular structures, combined with shared neural pathways and vascular supply, creates potential mechanisms for TMJ dysfunction to influence balance and spatial orientation.
Patients with TMJ-related vestibular symptoms often report that their dizziness or balance problems worsen with jaw movement or during episodes of increased muscle tension. Unlike vestibular disorders of inner ear origin, TMJ-related vestibular symptoms may respond to treatments targeting jaw dysfunction, providing both diagnostic and therapeutic insights. The relationship between TMJ disc displacement and vestibular symptoms represents an area of ongoing research, with emerging evidence suggesting stronger connections than previously recognised in clinical practice .
Diagnostic protocols for TMJ-Related otological complaints
Establishing an accurate diagnosis of TMJ-related ear symptoms requires a systematic approach that considers both the complexity of the temporomandibular system and the potential for symptom overlap with primary ear disorders. The diagnostic process must integrate clinical history, physical examination findings, imaging studies, and functional assessments to differentiate TMJ-induced ear complaints from other causes of auricular symptoms. This comprehensive approach is essential given that traditional ear examinations may appear completely normal in patients experiencing significant ear-related symptoms due to TMJ dysfunction.
The clinical history represents a crucial component of the diagnostic process, as TMJ-related ear symptoms often exhibit characteristic patterns that differ from those associated with primary ear pathology. Patients frequently report that their ear symptoms correlate with jaw activity, stress levels, or specific postures, providing important diagnostic clues. The temporal relationship between jaw dysfunction and ear symptoms, including any history of jaw trauma, dental procedures, or changes in bite relationship, should be carefully documented and considered in the diagnostic evaluation.
Physical examination protocols for suspected TMJ-related ear complaints must include both otological and temporomandibular assessments. The ear examination may reveal normal findings despite significant patient complaints, which itself can be diagnostically significant. Palpation of the temporomandibular joints during mouth opening and closing can reveal joint sounds, tenderness, or irregularities that suggest underlying dysfunction. Assessment of jaw movement patterns, including maximum mouth opening, lateral excursions, and protrusive movements, provides valuable information about joint function and muscle coordination.
Advanced imaging studies, including magnetic resonance imaging of the temporomandibular joints, can provide detailed information about disc position, joint morphology, and surrounding soft tissue structures. These imaging findings must be interpreted in the context of clinical symptoms, as asymptomatic individuals may exhibit imaging abnormalities, while some patients with significant symptoms may have relatively normal imaging findings. The correlation between imaging findings and clinical symptoms represents an important aspect of accurate diagnosis and treatment planning.
Effective diagnosis of TMJ-related ear symptoms requires clinicians to think beyond traditional anatomical boundaries and consider the complex interconnections between seemingly separate
systems.
Functional testing represents another crucial component of the diagnostic evaluation, with specific protocols designed to assess the relationship between jaw movement and auditory symptoms. These tests may include having patients perform specific jaw movements while monitoring for changes in ear pressure, tinnitus intensity, or hearing sensitivity. The presence of symptom modifications during these functional tests provides strong evidence for a TMJ-auditory connection and helps guide treatment planning decisions.
Collaborative assessment involving both dental and medical specialists often proves necessary for comprehensive evaluation of TMJ-related ear complaints. Otolaryngologists can rule out primary ear pathology, while TMJ specialists or orofacial pain specialists can assess the temporomandibular system’s contribution to symptoms. This multidisciplinary approach ensures that all potential causes of ear-related symptoms are properly evaluated and addressed in the treatment plan.
Evidence-based treatment approaches for TMJ-associated ear fullness
Effective management of TMJ-related ear fullness requires a comprehensive understanding of the underlying mechanisms and a systematic approach to treatment that addresses both the primary TMJ dysfunction and its secondary effects on auditory function. The evidence base for treating TMJ-associated ear symptoms continues to evolve, with research supporting various conservative and interventional approaches that can provide significant symptom relief when properly applied.
Conservative treatment approaches form the foundation of TMJ-related ear symptom management, with multiple studies demonstrating their effectiveness in reducing both jaw dysfunction and associated auricular complaints. Occlusal appliance therapy represents one of the most well-established treatments, with custom-fabricated oral splints helping to normalise jaw position and reduce muscle hyperactivity. These appliances work by creating optimal condylar positioning, which can alleviate pressure effects on nearby auditory structures and restore normal Eustachian tube function.
Physical therapy interventions specifically targeting TMJ dysfunction have shown considerable promise in addressing associated ear symptoms. Manual therapy techniques, including joint mobilisation, soft tissue manipulation, and trigger point release, can help restore normal jaw mechanics and reduce the muscular tension patterns that contribute to ear-related complaints. Exercise protocols focusing on jaw mobility, postural correction, and muscle strengthening provide patients with active management strategies that can prevent symptom recurrence.
Pharmacological interventions may be necessary in cases where inflammation or neuropathic pain mechanisms contribute significantly to symptom presentation. Anti-inflammatory medications can help reduce tissue swelling that may be impacting auditory structures, while neuropathic pain medications may be beneficial when nerve sensitisation or referred pain patterns are prominent. Muscle relaxants can provide temporary relief during acute exacerbations, though long-term management typically relies on addressing underlying mechanical dysfunction.
Advanced treatment modalities, including botulinum toxin injections and dry needling techniques, have emerged as valuable options for patients with persistent symptoms that do not respond adequately to conservative measures. These interventions target specific muscle groups or trigger points that contribute to both TMJ dysfunction and associated ear symptoms, often providing relief when traditional approaches have proven insufficient.
The integration of stress management and behavioural modification techniques represents a crucial component of comprehensive treatment, given that psychological stress often exacerbates both TMJ dysfunction and associated ear symptoms. Patients benefit from learning relaxation techniques, sleep hygiene protocols, and strategies for managing parafunctional habits such as teeth grinding or jaw clenching that can perpetuate their condition.
Treatment outcomes for TMJ-related ear symptoms are generally favourable when appropriate interventions are applied consistently and comprehensively. Many patients experience significant improvement in ear fullness, pressure sensations, and associated symptoms within weeks to months of initiating appropriate treatment. However, the complexity of TMJ-ear relationships means that treatment success often depends on addressing multiple contributing factors rather than focusing solely on isolated symptoms.
Long-term management strategies focus on maintaining the improvements achieved through initial treatment while preventing symptom recurrence. This typically involves ongoing use of occlusal appliances when indicated, maintenance of exercises and postural modifications learned during therapy, and regular monitoring to detect early signs of dysfunction recurrence. Patient education plays a vital role in long-term success, as individuals who understand the relationship between their jaw function and ear symptoms are better equipped to manage their condition effectively.
The prognosis for patients with TMJ-related ear fullness is generally positive, particularly when treatment addresses the underlying temporomandibular dysfunction rather than merely managing symptoms. Research indicates that comprehensive treatment approaches can provide lasting relief for the majority of patients, with many experiencing complete resolution of their ear-related complaints once normal jaw function is restored. However, the multifactorial nature of these conditions means that some patients may require ongoing management to maintain optimal symptom control.
Future directions in TMJ-ear relationship research continue to explore new treatment modalities and refine existing approaches. Emerging technologies, including neuromuscular re-education devices and advanced imaging techniques, promise to enhance both diagnostic accuracy and treatment effectiveness. As our understanding of these complex relationships continues to evolve, patients can expect increasingly sophisticated and effective treatment options for managing TMJ-associated ear symptoms.