The cervical transformation zone represents one of the most critical anatomical regions in women’s health, serving as the primary site where cervical neoplasia develops. This dynamic area, where squamous and glandular epithelium meet, undergoes continuous changes throughout a woman’s life, influenced by hormonal fluctuations, pregnancy, and various physiological factors. Understanding the significance of transformation zone presence in cervical screening has evolved considerably over the past decades, with recent research challenging long-held assumptions about specimen adequacy requirements. Modern evidence-based approaches now emphasise that the absence of transformation zone components in cervical samples does not necessarily indicate inadequate sampling or increased cancer risk, fundamentally reshaping how healthcare professionals interpret screening results.
Cervical transformation zone anatomy and histological characteristics
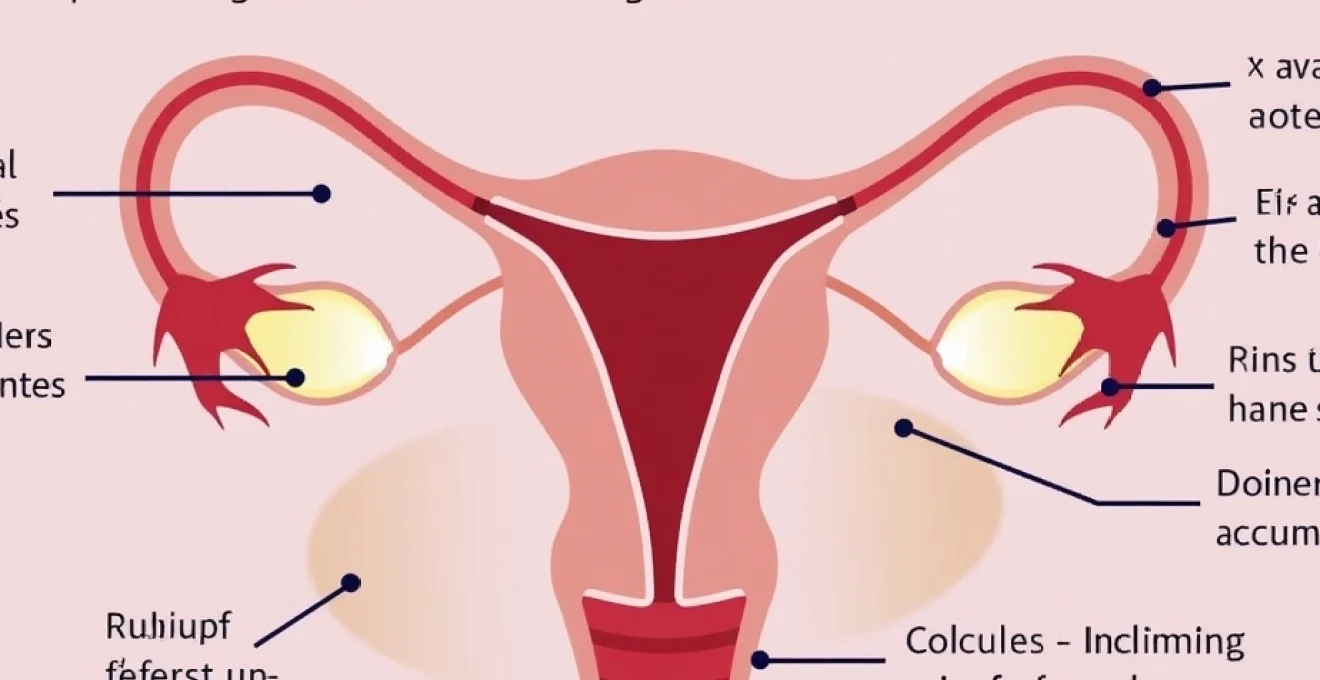
The transformation zone, often abbreviated as TZ, represents a unique anatomical region where the stratified squamous epithelium of the ectocervix meets the simple columnar epithelium of the endocervix. This junction, known as the squamocolumnar junction (SCJ), marks the boundary between two fundamentally different epithelial types, each with distinct cellular characteristics and vulnerability patterns. The transformation zone extends from the original squamocolumnar junction to the new squamocolumnar junction, encompassing an area of metaplastic squamous epithelium that has replaced the original columnar epithelium.
The histological composition of the transformation zone reveals a complex landscape of cellular activity. Metaplastic squamous epithelium within this region demonstrates varying degrees of maturation, often displaying reserve cell hyperplasia and immature squamous metaplasia. These cellular changes create an environment particularly susceptible to viral infections, most notably human papillomavirus (HPV), which explains why approximately 90% of cervical cancers originate within this specific anatomical region. The transformation zone’s unique cellular composition makes it an ideal target for both viral persistence and subsequent malignant transformation.
Squamocolumnar junction location and physiological variations
The location of the squamocolumnar junction varies significantly both between individuals and within the same person over time. During reproductive years, hormonal influences cause the junction to migrate inward and outward along the cervical canal, creating a dynamic boundary that responds to oestrogen and progesterone fluctuations. This physiological variation means that the transformation zone may be fully visible on the ectocervix during certain periods, whilst at other times it may be located entirely within the endocervical canal, invisible to direct visualisation.
Several factors influence the position of the squamocolumnar junction throughout a woman’s lifetime. Hormonal contraceptive use can cause the junction to migrate outward, making it more accessible during clinical examination. Conversely, the natural ageing process and declining oestrogen levels typically cause the junction to retreat into the endocervical canal, particularly following menopause. This migration pattern has significant implications for colposcopic examination and the ability to adequately assess the entire transformation zone during clinical procedures.
Metaplastic epithelium development during menarche and pregnancy
The development of metaplastic epithelium within the transformation zone undergoes significant changes during key reproductive milestones. During menarche, rising oestrogen levels cause the columnar epithelium to evert onto the ectocervix, exposing it to the acidic vaginal environment. This exposure triggers a process of squamous metaplasia, where reserve cells beneath the columnar epithelium proliferate and differentiate into squamous epithelium, gradually replacing the original glandular tissue.
Pregnancy represents a particularly active period for transformation zone modification. The hormonal environment during gestation causes extensive cervical remodelling, with the transformation zone often becoming more prominent and accessible. Pregnancy-related changes include increased vascularity, enhanced cellular proliferation, and accelerated metaplastic processes. These changes can make colposcopic interpretation more challenging, as pregnancy-related alterations may mimic pathological findings, requiring experienced assessment to distinguish between physiological and pathological changes.
Original squamocolumnar junction versus new squamocolumnar junction identification
Distinguishing between the original and new squamocolumnar junctions requires careful colposcopic examination and understanding of cervical development patterns. The original squamocolumnar junction represents the embryological boundary between the squamous and columnar epithelium, typically located at the external os in young women. However, hormonal influences throughout reproductive life cause this junction to migrate, leading to the formation of a new squamocolumnar junction at the current boundary between squamous and columnar epithelium.
The area between these two junctions constitutes the transformation zone, containing varying degrees of metaplastic squamous epithelium. Colposcopic landmarks help identify these boundaries, including the presence of nabothian cysts, gland openings, and characteristic vascular patterns. Accurate identification of both junctions is crucial for determining transformation zone types and assessing the adequacy of colposcopic examination, particularly when abnormalities are suspected within this high-risk region.
Transformation zone types classification according to IFCPC nomenclature
The International Federation for Cervical Pathology and Colposcopy (IFCPC) has established a standardised classification system for transformation zone types, providing consistent terminology for clinical documentation and research purposes. This classification system recognises three distinct transformation zone types based on the visibility and accessibility of the squamocolumnar junction and transformation zone boundaries during colposcopic examination.
Type 1 transformation zones are completely visible on the ectocervix, with both the original and new squamocolumnar junctions clearly identifiable without the need for endocervical visualisation. Type 2 transformation zones have a new squamocolumnar junction that extends into the endocervical canal but remains visible with appropriate speculum placement and colposcopic technique. Type 3 transformation zones present the greatest challenge, with the new squamocolumnar junction located entirely within the endocervical canal, beyond the limits of standard colposcopic visualisation. This classification system helps standardise reporting and ensures appropriate management decisions based on the accessibility of the transformation zone for adequate assessment.
Colposcopic assessment techniques for transformation zone visualisation
Colposcopic examination represents the gold standard for detailed transformation zone assessment, providing magnified visualisation and enabling the application of various enhancement techniques to reveal subtle abnormalities. The systematic approach to colposcopic assessment begins with low magnification examination to identify the transformation zone boundaries and overall cervical architecture. Progressive magnification allows for detailed evaluation of surface patterns, vascular architecture, and colour changes that may indicate underlying pathology. The quality of colposcopic assessment directly impacts the accuracy of abnormality detection and the appropriateness of subsequent management decisions.
Modern colposcopic techniques emphasise the importance of adequate transformation zone visualisation for comprehensive cervical assessment. The inability to visualise the entire transformation zone may necessitate additional procedures, such as endocervical curettage or cone biopsy, to ensure complete evaluation of high-risk areas. However, recent evidence suggests that the clinical significance of invisible transformation zones may be less concerning than previously thought, particularly when high-risk HPV testing is negative and there is no history of previous cervical abnormalities.
Acetic acid application protocol and acetowhite epithelium recognition
The application of 3-5% acetic acid solution represents a fundamental component of colposcopic examination, causing reversible coagulation of nuclear proteins in abnormal epithelium. This process results in the characteristic acetowhite appearance that helps identify areas of increased nuclear density, typically associated with dysplastic changes. Proper acetic acid application requires thorough coverage of the entire transformation zone and adjacent areas, followed by systematic examination during the optimal viewing period of 30-60 seconds after application.
The interpretation of acetowhite changes requires careful attention to the intensity, rapidity of appearance, and persistence of the colour change. Dense acetowhite epithelium with sharp borders typically indicates higher-grade abnormalities, whilst faint or slowly developing acetowhite changes may represent low-grade lesions or metaplastic epithelium. The ability to distinguish between significant acetowhite changes and physiological variations comes with experience and forms the cornerstone of accurate colposcopic assessment. Geographic patterns of acetowhite epithelium within the transformation zone help guide biopsy decisions and treatment planning.
Lugol’s iodine staining patterns and schiller test interpretation
Lugol’s iodine application provides complementary information to acetic acid assessment, utilising the glycogen content of normal squamous epithelium to create distinctive staining patterns. Normal mature squamous epithelium contains abundant glycogen and stains dark brown with iodine, whilst abnormal epithelium typically shows reduced or absent glycogen, resulting in non-staining or mustard-yellow areas. The Schiller test helps delineate the extent of abnormal areas and can be particularly useful when acetowhite changes are subtle or when determining the margins of lesions for treatment planning.
Interpretation of iodine staining requires understanding of physiological variations that can affect glycogen content. Inflammatory conditions, metaplastic epithelium, and hormonal influences can all result in reduced glycogen and subsequent non-staining patterns that do not necessarily indicate dysplasia. The combination of acetic acid and iodine findings provides a more comprehensive assessment than either test alone, helping to distinguish between inflammatory, metaplastic, and dysplastic changes within the transformation zone.
Green filter enhancement for vascular pattern analysis
Green filter colposcopy enhances the visualisation of cervical vasculature by improving contrast between blood vessels and surrounding epithelium. This technique proves particularly valuable for identifying abnormal vascular patterns associated with high-grade lesions and invasive cancer. Vascular pattern analysis includes assessment of intercapillary distances, vessel calibre variations, and architectural arrangements that may indicate underlying pathology. The recognition of atypical vessels, including punctation, mosaic patterns, and atypical vessels associated with invasion, requires systematic training and experience.
The integration of green filter examination into routine colposcopic assessment enhances the detection of subtle vascular abnormalities that may not be apparent with standard white light examination. This technique is particularly useful when evaluating areas of dense acetowhite epithelium where surface features may obscure underlying vascular patterns. The ability to characterise vascular abnormalities accurately contributes to more precise colposcopic impression formation and appropriate biopsy targeting.
Digital colposcopy documentation standards and image capture protocols
Digital colposcopy systems have revolutionised documentation standards and enable comprehensive image archival for quality assurance, medicolegal purposes, and educational activities. Standardised image capture protocols should include documentation of the transformation zone before and after acetic acid application, green filter examination of vascular patterns, and post-iodine staining appearances. High-resolution digital images allow for detailed review, consultation with colleagues, and longitudinal comparison during follow-up examinations.
The implementation of digital colposcopy documentation requires adherence to established protocols that ensure consistent image quality and comprehensive coverage of relevant findings. Sequential image capture following a systematic protocol helps avoid missing important areas and provides a complete visual record of the examination. Digital systems also facilitate the integration of artificial intelligence tools that may assist in pattern recognition and quality assurance, representing an evolving area of technological advancement in colposcopic practice.
Hpv-related cellular changes within the transformation zone
The transformation zone’s unique cellular composition creates an optimal environment for human papillomavirus infection and persistence. The metaplastic epithelium within this region demonstrates increased susceptibility to viral integration due to active cellular proliferation and the presence of immature squamous cells. HPV-induced cellular changes manifest as a spectrum of morphological alterations, ranging from subtle koilocytotic changes in low-grade lesions to severe nuclear abnormalities in high-grade dysplasia. Understanding these cellular modifications is crucial for interpreting both cytological and histological findings within the transformation zone context.
Recent molecular studies have revealed that high-risk HPV types demonstrate preferential integration sites within the transformation zone, with viral load and integration patterns influencing the likelihood of progression to invasive cancer. The interaction between HPV oncoproteins and cellular tumour suppressor pathways creates a cascade of molecular events that drive dysplastic progression. Viral persistence within the transformation zone correlates strongly with the development of high-grade lesions, explaining why HPV testing has become an essential component of modern cervical screening programmes.
The cellular changes induced by HPV infection extend beyond morphological alterations to include epigenetic modifications and alterations in cellular differentiation pathways. The transformation zone’s unique microenvironment, characterised by hormonal influences, immune surveillance patterns, and microbiome composition, modulates viral persistence and progression risk. These complex interactions explain why some HPV infections resolve spontaneously whilst others progress to invasive cancer, highlighting the importance of understanding transformation zone biology in cervical cancer prevention strategies.
Modern research has identified specific biomarkers associated with HPV-induced transformation zone changes, including p16 overexpression, Ki-67 proliferation indices, and viral integration patterns. These molecular markers enhance diagnostic accuracy and provide prognostic information beyond traditional morphological assessment. Biomarker-assisted interpretation of transformation zone abnormalities represents a rapidly evolving field that promises to improve both diagnostic precision and risk stratification in cervical screening programmes.
Cervical screening programme integration and cytological correlation
Modern cervical screening programmes have evolved to incorporate sophisticated understanding of transformation zone biology and its relationship to specimen adequacy. The historical emphasis on transformation zone presence as a marker of specimen quality stemmed from early studies that suggested increased cancer risk when endocervical cells were absent from cytological samples. However, contemporary evidence-based research has fundamentally challenged these assumptions, demonstrating that the absence of transformation zone components does not necessarily indicate inadequate sampling or increased cancer risk.
The integration of HPV testing into cervical screening programmes has provided new insights into the relationship between transformation zone sampling and cancer detection rates. Studies consistently demonstrate that high-risk HPV detection remains effective regardless of transformation zone presence in cytological specimens. This finding has significant implications for screening programme efficiency, as it suggests that repeat testing solely based on absent transformation zone components may not represent cost-effective healthcare delivery.
NHS cervical screening programme protocol adherence for transformation zone sampling
The NHS Cervical Screening Programme has implemented evidence-based protocols that reflect current understanding of transformation zone significance in screening effectiveness. These protocols emphasise the importance of adequate sampling technique whilst acknowledging that transformation zone presence is not an absolute requirement for specimen adequacy. Sample collection protocols focus on obtaining representative cellular material from the cervical surface and endocervical canal using appropriate collection devices and techniques that maximise cellular yield.
Training programmes for healthcare professionals emphasise proper sampling technique, including the use of appropriate spatulas and brushes, adequate pressure application, and systematic coverage of the cervical surface. The protocols recognise that anatomical variations, particularly in postmenopausal women, may make transformation zone sampling challenging or impossible without causing unnecessary discomfort. Quality assurance measures focus on overall sample adequacy rather than specifically requiring transformation zone presence, reflecting current evidence-based understanding.
Liquid-based cytology collection techniques from adequate transformation zone
Liquid-based cytology has become the standard collection method in many screening programmes, offering advantages in cellular preservation, sample adequacy, and the ability to perform reflex HPV testing from the same specimen. Collection techniques for liquid-based cytology require specific attention to cellular transfer efficiency and preservation of morphological detail. The technique involves thorough mixing of collected cellular material in preservative solution, ensuring optimal cellular dispersion and fixation for subsequent processing.
The adequacy criteria for liquid-based cytology specimens have evolved to reflect current understanding of transformation zone significance. Modern adequacy assessment focuses on overall cellular yield, presence of squamous epithelial cells, and absence of obscuring factors such as excessive inflammation or blood. The presence of endocervical cells, whilst desirable, is not considered essential for specimen adequacy when adequate squamous cellularity is achieved and clinical risk factors are appropriate.
HPV primary screening implementation and triage pathways
The implementation of HPV primary screening has revolutionised cervical cancer prevention by focusing on the detection of causative viral infection rather than morphological changes alone. HPV-based screening protocols demonstrate superior sensitivity for high-grade lesions and invasive cancer whilst maintaining acceptable specificity through appropriate triage mechanisms. This approach is particularly relevant to transformation zone assessment, as HPV detection effectiveness appears independent of endocervical cell presence in screening samples.
Triage pathways for HPV-positive women incorporate cytological assessment and risk stratification based on age, HPV type, and previous screening history. The protocols recognise that transformation zone-specific sampling may not be necessary for effective cancer prevention when appropriate risk assessment and follow-up procedures are implemente
d. These pathways acknowledge that transformation zone sampling considerations should be balanced against patient comfort and clinical necessity, particularly when alternative risk assessment methods are available.
Bethesda system reporting standards for transformation zone adequacy
The Bethesda System for Reporting Cervical Cytology has evolved to reflect current evidence regarding transformation zone adequacy requirements. Modern reporting standards recognise that specimen adequacy assessment should encompass multiple factors beyond simple endocervical cell presence. Contemporary adequacy criteria focus on overall sample quality, including adequate cellularity, appropriate fixation, and absence of obscuring factors that might compromise diagnostic interpretation. The system acknowledges that transformation zone absence does not automatically render a specimen inadequate for diagnostic purposes.
Current Bethesda guidelines emphasise that endocervical cells serve as an indicator of sampling from the transformation zone area but are not an absolute requirement for specimen adequacy. The guidelines recognise anatomical and physiological factors that may limit transformation zone sampling, including age-related changes, previous procedures, and individual anatomical variations. Quality indicators now focus on technical adequacy and cellular preservation rather than specific cell type representation, reflecting improved understanding of screening effectiveness and cancer detection rates.
The reporting framework incorporates risk-stratified approaches that consider clinical context alongside cytological findings. When transformation zone components are absent, the reporting includes appropriate qualifiers that guide clinical management decisions. This approach ensures that healthcare providers receive relevant information for patient counselling whilst avoiding unnecessary anxiety about specimen adequacy when clinical risk factors suggest routine screening intervals remain appropriate.
Educational initiatives accompanying Bethesda System implementation emphasise the importance of clinical correlation and risk assessment in interpreting cytological reports. The system promotes understanding among healthcare providers that transformation zone absence should be interpreted within the broader clinical context, including patient age, screening history, and concurrent HPV testing results. Evidence-based reporting standards help ensure that cytological interpretation aligns with current scientific understanding of cervical cancer prevention and screening effectiveness.
Pathological conditions associated with transformation zone abnormalities
The transformation zone serves as the epicentre for various pathological conditions affecting the cervix, with its unique cellular composition and hormonal responsiveness creating vulnerability to multiple disease processes. Cervical intraepithelial neoplasia represents the most clinically significant abnormality arising within this region, encompassing a spectrum of dysplastic changes that may progress to invasive carcinoma if left untreated. Pathological processes within the transformation zone often reflect the complex interplay between viral infections, hormonal influences, and host immune responses, creating diverse clinical presentations that require expert interpretation and management.
Inflammatory conditions frequently affect the transformation zone, particularly during periods of hormonal change or immune compromise. Chronic cervicitis may develop within areas of active metaplasia, creating diagnostic challenges when attempting to distinguish between inflammatory and dysplastic changes. The presence of repair processes, reactive cellular changes, and inflammatory infiltrates can complicate cytological and histological interpretation, requiring correlation with clinical findings and HPV testing results to ensure accurate diagnosis and appropriate management decisions.
Infectious processes beyond HPV commonly involve the transformation zone, including bacterial, fungal, and parasitic infections that may alter normal cellular architecture and function. Candidal infections can cause significant inflammatory changes that mimic dysplastic alterations on both cytological and colposcopic examination. Bacterial vaginosis and other vaginal infections may create inflammatory responses that extend to the transformation zone, potentially affecting screening test interpretation and requiring treatment before definitive assessment of underlying cervical abnormalities can be performed.
Benign epithelial abnormalities within the transformation zone include various forms of metaplastic change that may appear concerning on routine screening but represent normal physiological processes. Immature squamous metaplasia can demonstrate cellular atypia that may be misinterpreted as dysplastic change, particularly when inflammatory processes are concurrent. Understanding the spectrum of benign changes helps prevent overdiagnosis and inappropriate treatment whilst ensuring that genuinely abnormal findings receive appropriate attention and management. The development of biomarker testing has enhanced diagnostic accuracy by providing objective measures to distinguish between reactive and dysplastic changes within the transformation zone.
Clinical management strategies for transformation zone lesions
Contemporary clinical management of transformation zone lesions emphasises risk-stratified approaches that consider multiple factors including lesion grade, HPV status, patient age, and previous screening history. The evolution from uniform treatment protocols to personalised management strategies reflects improved understanding of natural history and progression risks associated with different lesion types. Conservative management has gained acceptance for low-grade lesions, particularly in younger women where spontaneous regression rates are high and treatment-related morbidity may outweigh benefits. This approach requires robust follow-up protocols and patient education to ensure appropriate monitoring and timely intervention when progression occurs.
Treatment selection for high-grade transformation zone lesions involves careful consideration of multiple factors including lesion extent, colposcopic findings, pregnancy status, and patient preferences. Large loop excision of the transformation zone (LLETZ) remains the most commonly employed treatment modality, offering both diagnostic and therapeutic benefits through complete lesion excision with histological margin assessment. Cold knife conisation may be preferred when precise margin evaluation is crucial or when glandular abnormalities are suspected, despite higher morbidity rates compared to electrosurgical techniques.
Ablative treatment methods, including cryotherapy and laser ablation, provide alternatives for selected cases where complete lesion destruction is acceptable and histological confirmation of excision margins is not essential. These techniques require careful patient selection and thorough pre-treatment assessment to ensure complete transformation zone coverage and absence of invasive disease. Follow-up protocols following ablative treatments must be particularly rigorous given the inability to assess treatment margins histologically, typically involving more frequent surveillance and lower thresholds for repeat intervention.
Emerging treatment modalities include immunomodulatory therapies and targeted antiviral treatments that may offer less invasive alternatives for managing transformation zone abnormalities. Research into therapeutic HPV vaccines and immune enhancement strategies shows promise for treating persistent infection and preventing progression to high-grade disease. Personalised medicine approaches incorporating genetic markers, viral load assessment, and immune status evaluation may soon enable more precise treatment selection and improved outcomes for women with transformation zone abnormalities. The integration of artificial intelligence and machine learning tools into diagnostic and treatment algorithms represents an exciting frontier that may enhance both accuracy and efficiency in managing cervical abnormalities within the transformation zone.